Maintenance therapy with PARP inhibitor olaparib delays progression of BRCA-related pancreatic cancer
2019 ASCO Annual Meeting News Release Jun 06, 2019
The randomized, phase III POLO trial found that maintenance therapy with the PARP inhibitor olaparib (Lynparza) significantly delayed the progression of metastatic pancreatic cancer in patients with BRCA gene mutations compared with placebo (median progression-free survival: 7.4 months vs. 3.8 months, respectively). In the trial, olaparib was administered to patients with cancer that had not progressed after completion of initial platinum-based chemotherapy, and after two years, 22.1% of people receiving olaparib had no disease progression vs. 9.6% for those treated with placebo. While overall survival data are not yet mature, this is a significant advance given that the median survival of metastatic pancreatic cancer is currently less than one year.
ASCO Perspective
“We are eagerly awaiting longer-term data to understand the full impact of the results from this trial. It’s encouraging to see that olaparib is consistently delaying the progression of metastatic pancreatic cancer in patients with a BRCA mutation. We’re potentially on the cusp of a new age of treatment for pancreatic cancer, where for the first time we can tailor therapy based on a biomarker and where having a BRCA mutation opens up more treatment options,” said Suzanne Cole, MD.
These findings was presented in ASCO’s Plenary Session, which features four studies of great importance to patient care, out of the 5,600 abstracts accepted to the 2019 American Society of Clinical Oncology (ASCO) Annual Meeting.
“POLO is the first phase III randomized study to establish a biomarker-driven approach in the treatment of metastatic pancreatic cancer, and it opens the door to a new era of personalized care for this difficult-to-treat cancer,” said lead study author Hedy L. Kindler, MD, FASCO, Professor of Medicine, University of Chicago Medicine. “Roughly one in five patients responded to olaparib for a median of two years, which is truly remarkable for metastatic pancreatic cancer. For patients with BRCA-driven metastatic pancreatic cancer, we may be seeing a change in patients’ disease trajectory.”
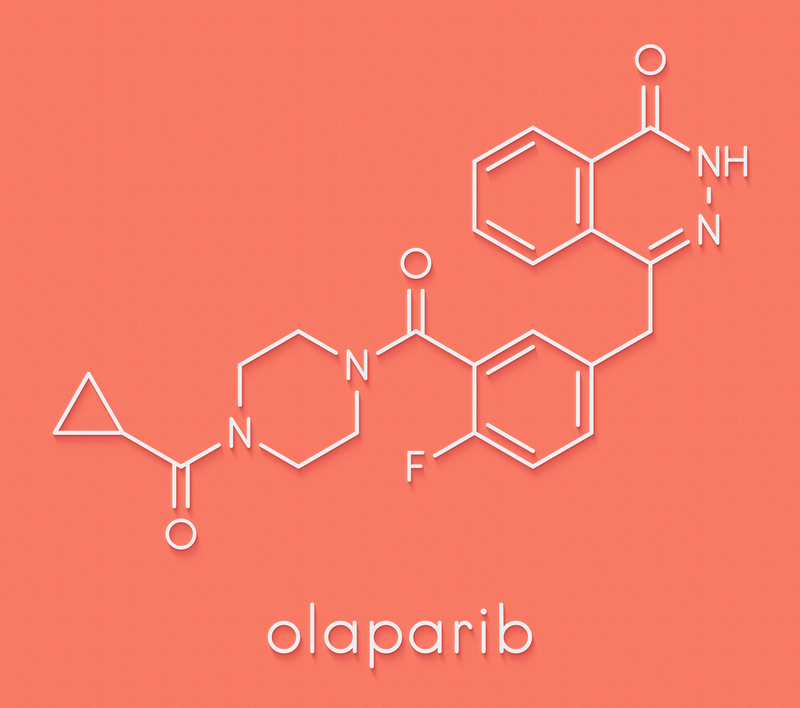
Olaparib is a targeted therapy that inhibits PARP enzymes, which are important in DNA transcription and repair. Olaparib is currently approved by the U.S. Food and Drug Administration as first-line maintenance treatment in patients with BRCA mutations who benefitted from prior platinum-based chemotherapy.
Germline BRCA mutations are inherited and are known to increase the chances of developing several other cancers, including ovarian, breast, and prostate cancer. Previous phase III studies have to date shown the benefit of olaparib in other BRCA-driven cancers (ovarian, breast). About 5% to 6% of pancreatic cancers are caused by mutations in one or both BRCA genes.[1]
In January 2019, ASCO issued a Provisional Clinical Opinion (PCO) recommending that people with pancreatic cancer undergo risk assessment for hereditary syndromes that increase pancreatic cancer risk. The PCO also states that germline genetic testing for cancer susceptibility – including testing for BRCA mutations – may be discussed with individuals diagnosed with pancreatic cancer, even if family history does not clearly suggest an inheritable cancer-related syndrome.
About the Study
The current trial builds on phase II data from a 2015 trial[2] finding 22% response rates (tumor shrinkage) in pancreatic cancers with BRCA1/2 gene mutations treated with olaparib, following chemotherapy with gemcitabine (Gemzar). The POLO trial examined if olaparib could delay disease progression after 16 weeks or more of initial platinum-based chemotherapy. Toxicities to platinum-based chemotherapy often increase the longer they are taken, so some people stop the medicines after 16 weeks. The use of an oral, non-chemotherapeutic medicine with lower toxicities, such as olaparib, would provide an important option, according to the authors.
After screening 3,315 people with pancreatic cancer, the investigators identified 247 with germline BRCA mutations. The researchers randomly assigned 154 patients on a 3:2 basis, with 92 people assigned to olaparib and 62 assigned to placebo. Treatment started 4 to 8 weeks after a patient’s last dose of platinum-based chemotherapy. The median duration of treatment was 6 months for those taking olaparib and 3.7 months for people who received a placebo.
Enrollees were a median age of 57; 58% of the people who received olaparib were men and equal numbers of men and women received placebo. Two-thirds of those enrolled had BRCA2 mutations, and the remainder had BRCA1mutations.
Key Finding
Patients were initially evaluated for disease progression every 8 weeks, then subsequently for 40 weeks, and every 12 weeks thereafter. At 6, 12, 18, and 24 months after the investigators randomly assigned people to a treatment, those who received olaparib were at least twice as likely to have no disease progression compared with those who received placebo.
Olaparib reduced the risk of disease progression by 47% (Hazard ratio = 0.53) compared with those getting a placebo. The median progression-free survival for patients receiving olaparib was 7.4 months, compared with 3.8 months for patients who received a placebo. After one year, 33.7% of patients receiving olaparib showed no signs of disease progression compared with 14.5% of those who received a placebo. After two years, 22.1% of people receiving olaparib had no cancer progression compared with 9.6% of those receiving a placebo.
Serious side effects (grade 3, 4, or 5) occurred in 40% of people taking olaparib compared with 23% of those taking a placebo. In addition, 5.5% of those taking olaparib and 1.7% of those on placebo discontinued treatment due to toxicity. Olaparib was well tolerated and there was no difference in quality of life between those taking olaparib and placebo.
Next Steps
Dr. Kindler notes that the results of this trial are likely practice-changing. The long-term goal is to demonstrate the utility of olaparib in pancreatic cancer beyond the patients who benefitted from the medicine in the POLO trial.
This study received funding from AstraZeneca and Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA.
This article is a news release from 2019 ASCO Annual Meeting. Read the original here.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries