Congestion at discharge worsens prognosis for patients with AHF: Results from the ESC EORP Heart Failure Long-Term Registry
Heart Failure 2019 Congress News May 31, 2019
Classifying patients with acute heart failure according to congestion/ hypoperfusion provides clinically relevant information both at hospital admission and at discharge.
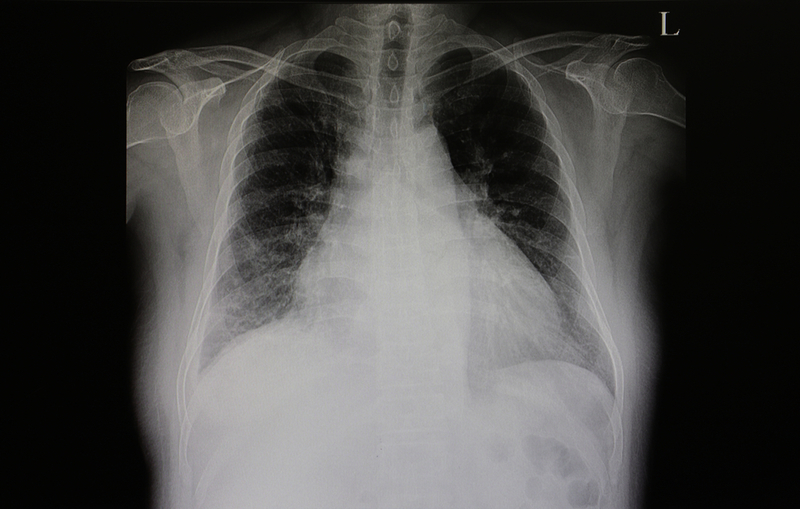
This is according to a late-breaking trial presentation yesterday by Doctor Ovidiu Chioncel (Emergency Institute for Cardiovascular Disease “Prof C.C. Iliescu”, Bucharest, Romania) (LBT9). Dr. Chioncel outlines the problem of classification, explaining that because of the diverse nature of acute heart failure and the heterogeneity of its signs and symptoms, a standard means of classifying patients that can be applied globally is required to enable optimum management of the condition. The study retrospectively applied the congestion (wet or dry)/hypoperfusion (cold or warm) categories from the ESC 2016 Guidelines for the diagnosis and treatment of acute and chronic heart failure to data from 7,865 patients with acute heart failure from the EURObservational Heart Failure Long-Term Registry, both at hospital admission and hospital discharge. The dataset covers a broad range of individuals with acute heart failure, including patients with any ejection fraction level, and was obtained from large multicentre registries that collected data systematically in a wide range of European and non-European countries.
At admission, patients were classified as ‘drywarm’ (9.9%), ‘wet-warm’ (69.9%), ‘wet-cold’ (19.8%) and ‘dry-cold’ (0.4%). In-hospital mortality was 2.0% in ‘dry-warm’, 3.8% in ‘wet-warm’, 9.1% in ‘dry-cold’ and 12.1% in ‘wet-cold’ patients.
In a Cox-proportional hazard model with multivariable adjustment, based on classification at admission, ‘wet-warm’ was not worse than ‘dry-warm’ for in-hospital mortality, suggesting that congestion can be addressed in hospital. However, hypoperfusion on admission was associated with in-hospital mortality. Using classification at discharge, both hypoperfusion and congestion were associated with one-year mortality. Nearly one-third (30.9%) of patients with acute heart failure discharged from hospital had residual congestion.
One-year mortality was higher in patients with vs without congestion at discharge (28.0% vs 18.5%).
The finding regarding congestion is particularly important, according to Dr. Chioncel. “Congestion on discharge, even to a minor degree, is associated with poor prognosis and treatment of residual congestion should be addressed as a matter of priority. The classification system may help to ensure that congestion, which may otherwise be overlooked, is identified and can be managed appropriately.” He recognises that while the congestion/hypoperfusion system is a big step forward in standardising classification, it cannot be used in isolation. Instead, it should be supported by information from biological variables, such as natriuretic peptic levels, particularly in patients without evident clinical signs of congestion. He also acknowledges that clinical signs of hypoperfusion are not well understood and that doctors may only be aware of it following cardiogenic shock. “There needs to be greater understanding of hypoperfusion so that it is possible to anticipate and prevent a potential cardiogenic shock,” he says.
This article is a news release from Heart Failure 2019 Congress. Read the original here.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries