Viral Fever: Understanding, Managing, and Preventing Seasonal Flu
M3 India Newsdesk Jun 26, 2024
This article focuses on respiratory infections like the seasonal flu and discusses the causes, symptoms, indicators, and prevention of viral fevers. To control and lessen the effects of these infections, it emphasises diagnostic techniques, available treatments, and preventive measures.
A temperature of >37.7 0 C (>99.90F), which represents the 99th percentile for healthy individuals, defines a fever. Whatever raises a fever is referred to as pyrogen. Exogenous pyrogens originate from sources external to the body; the majority are poisons or products of microbes, including viruses.
Fevers, especially seasonal flu, are common afflictions affecting millions worldwide each year. They present a significant health concern due to their contagious nature and potential for complications.
Understanding the causes, signs, and symptoms of viral fevers is crucial for effective management and prevention, particularly in the case of seasonal flu.
Causes of viral fever
Viral fevers are primarily caused by viral infections. Various viruses, including influenza viruses (Orthomyxoviridae), rhinoviruses, adenoviruses, and coronaviruses, are responsible for triggering these fevers. Seasonal flu, caused by influenza viruses, tends to peak during specific times of the year, typically during colder months.
A range of different viruses can cause RTIs²; the most common viruses implicated are:
- Orthomyxoviridae: Influenza viruses
- Paramyxoviridae: Respiratory syncytial virus (RSV), parainfluenza virus (PIV) 1-4, and human metapneumovirus (hMPV)
- Coronavirus
- Picornaviruses: Enteroviruses and parechoviruses.
The incubation period and seasonality of these individual viruses vary (Tables 1 and 2). These viruses are predominantly transmitted by droplet transmission and by fomites. Airborne transmission is possible particularly ventilated patients and patients undergoing aerosol-generating procedures (e.g., influenza).
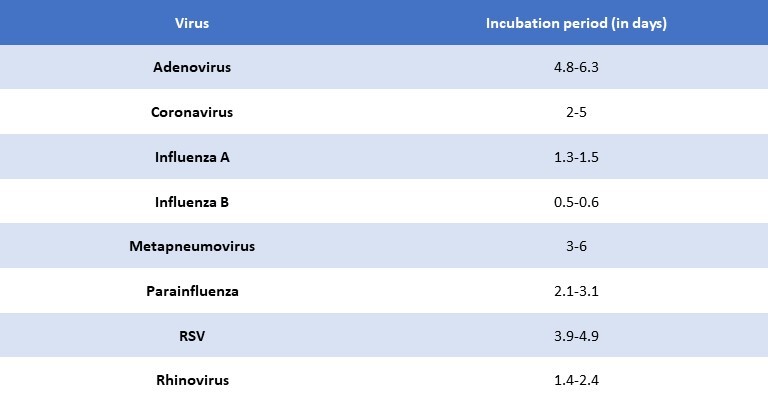
TABLE 1: Viruses and incubation period.
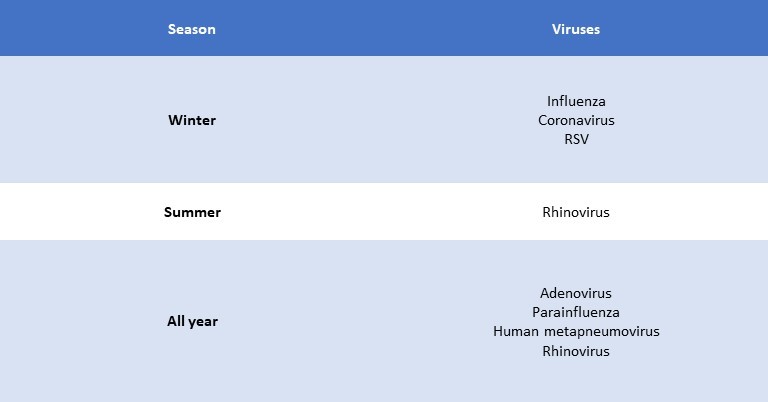
TABLE 2: Seasonality of viruses
Signs and symptoms
The symptoms of viral fevers, including seasonal flu, can vary but often include:
1. Fever: Elevated body temperature is a hallmark symptom of viral fevers. It may range from mild to high-grade, accompanied by chills.
2. Cough: Dry or productive coughing is common, especially with respiratory viral infections like flu.
3. Sore throat: Irritation or pain in the throat may occur due to inflammation.
4. Fatigue: Profound tiredness and weakness are often reported, impacting daily activities.
5. Muscle aches: Generalised muscle pain and body aches are frequent complaints.
6. Headache: Intense headaches, sometimes accompanied by sinus pressure, are typical.
7. Nasal congestion: Blocked or runny nose is common, particularly with respiratory virus
Clinical manifestations
1. Influenza
- Influenza viruses are the most common respiratory viruses causing m outbreaks of varying severity and leading to excess morbidity. There are two types of viruses, types A and B that cause the illness, Influenza is usually associated with a U-shaped epidemic curve, with attack rates being highest in the young and mortality higher among the elderly. Patients with underlying medical conditions, pregnancy, and obesity are at increased risk.
- After an incubation period of 1-2 days, typical uncomplicated influenza frequently starts with a rapid onset of symptoms. Systemic symptoms such as fever, chills, headache, myalgia, malaise, and anorexia predominate and persist for 3 days. Respiratory symptoms include a dry cough, severe pharyngeal pain, nasal obstruction, and discharge.
- The patient appears toxic with flushing of the face. The mucous membranes of the nose and throat are hyperaemic and nasal discharge is clear. Crackles and wheeze may be found occasionally. Then, a convalescent period of 1 or more weeks to full recovery ensues.
- Bacterial superinfection is a well-recognised complication of influenza and accounts for a substantial proportion of the morbidity and mortality of the disease. The continuous evolution and reassortment of these viruses remain a cause for concern warranting continuous monitoring and surveillance.
2. Respiratory syncytial virus
- The primary cause of lower respiratory tract infections in young children is the respiratory syncytial virus. Essentially all persons get infected with RSV within the first few years of life. RSV is also of concern in elderly people >65 years particularly in people with cardiopulmonary disease.
- The respiratory syncytial virus is the most frequent cause of bronchiolitis constituting 40-90% of the hospitalised cases and 50% of pneumonia in infants. Croup and tracheobronchitis are the other clinical manifestations.
- Preterm gestation, with or without underlying chronic lung disease or congenital heart disease, is a major risk factor for more severe RSV disease.
- In young children, it is confined to the upper respiratory tract and otitis media can occur. Recurrent wheeze is a known sequela in children.
- Among healthy adults, following RSV infection, 84% were symptomatic and 22% had lower respiratory tract manifestations similar to influenza. Among older individuals, RSV is remarkably identical to influenza concerning clinical manifestations and as a cause of hospitalisation. Though reinfections are common in all age groups, they tend to be less severe.
3. Parainfluenza
- Human PIVs cause a mild and self-limiting illness predominantly; however, life-threatening lower RTIs do occur, particularly in the elderly and immunocompromised.
- The second most frequent viral cause of pediatric hospitalisation is parainfluenza. Human PIV is of four types. PIV-1 and PIV-2 cause seasonal outbreaks in winter and PIV-3 causes epidemics in summer.
- A range of upper and lower respiratory tract infections, from minor cold-like symptoms to potentially fatal pneumonia, are caused by parainfluenza viruses.
- Infections in children are limited to the upper respiratory tract, with otitis media and sinusitis occurring in 30-50% and 15% having a lower respiratory tract involvement. PIV-3 and PIV-4 are linked to pneumonia and bronchiolitis in children, PIV-1 and PIV-2 to croup, or laryngotracheobronchitis, and PIV-4 to mild upper respiratory infections.
- In adults, PIV-3 causes influenza-like illness. PIV is also increasingly associated with exacerbations of asthma and chronic bronchitis. Meningitis, myocarditis, pericarditis, and Guillain-Barré syndrome are rare extrapulmonary complications.
4. Human metapneumovirus
- Human metapneumovirus more commonly occurs as a coinfection with other viral and bacterial respiratory pathogens. Seroprevalence studies indicate that 50% are seropositive by 2 years and 100% by 5 years of age. Outbreaks of hMPV usually alternate with RSV activity.
- Most young children with hMPV infection exhibit fever, cough, and rhinorrhoea. Fever appears to be more common and febrile seizures are noted in 16% of patients.
- Apart from conjunctivitis, pharyngitis, and laryngitis, wheezing and acute otitis media do occur. Neurologic complications, such as seizures, ataxia, and encephalitis, appear to be 10 times more common in children with hMPV, Maculopapular rash and diarrhoea are the other manifestations.
- In healthy adults, hMPV generally presents with mild Influenza-like illness and common cold syndromes. Hoarseness of voice is more common and occasionally a mononucleosis-like syndrome has been reported.
- Laboratory findings are nonspecific. Lymphopenia and elevated hepatic transaminases have been described. Radiographic findings include peribronchial cuffing, perihilar infiltrates, patchy opacities, and hyperinflation. In adults, patchy, multilobe infiltrates associated with small pleural effusions are noted in 50% of cases.
5. Coronavirus
- Coronaviruses are subclassified into four genera, among which human coronavirus (HCoVs) belong to two groups: Alpha coronaviruses (HCoV 229E and HCoV-NL63) and beta coronaviruses [HCoV-HKUI, HCOV-OC43, Middle East respiratory syndrome coronavirus (MERS-CoV), the severe acute respiratory syndrome coronavirus (SARS-CoV), and SARS-CoV2].
- Coronavirus accounts for 5-10% of cases of the common cold. Asymptomatic infection does occur. It is also implicated as a cause of acute otitis media.
- Coronavirus causes pneumonia similar to or somewhat lower than other respiratory viruses such as influenza, RSV, and rhinovirus. They have been found to cause exacerbations of chronic obstructive pulmonary disease and are also temporally linked to acute asthma attacks in both children and adults.
- SARS was characterised by fever and myalgia rapidly progressing to a respiratory syndrome of cough and dyspnea followed by acute respiratory distress syndrome. More mild and asymptomatic cases are observed with MERS, and mortality is strongly associated with age and comorbidities.
- SARS-CoV-2 has a similar clinical picture with initial upper respiratory or gastrointestinal symptoms along with fever and myalgia progressing to pneumonia in selected patients.
6. Adenovirus
- Adenovirus usually causes mild, self-limiting disease. Infections are more common in childhood and by 10 years of age, many are serologically positive. Almost 50% of individuals may have a subclinical infection and sporadic outbreaks are more common.
- There are several subtypes. Children may present with mild pharyngitis or tracheitis. It is usually associated with types 1, 2, 5, and 6 and rarely 3 and 7.
- It is at times indistinguishable from Group A streptococcal pharyngitis.
- Types 1-5, 7, 14, and 21 are associated with pneumonia. Severe, complicated pneumonia is reported with virus types 3, 7, 14, and 21. A frequent presentation of pharyngoconjunctival fever includes benign follicular conjunctivitis, fever pharyngitis, and cervical adenitis, all of which are brought on by adenovirus types 3 and 7.
- Other clinical manifestations include acute gastroenteritis, mesenteric adenitis, and hemorrhagic cystitis. Extrapulmonary complications occur rarely and include meningoencephalitis, hepatitis, myocarditis, nephritis, neutropenia, and disseminated intravascular coagulopathy, particularly in immunocompromised patients.
7. Rhinovirus
- Among the most frequent infections that affect people are rhinoviruses. They are the most important cause of the common cold and are implicated in 30-50% of all cases of acute respiratory disease.
- Rhinovirus colds frequently begin as a sore or "scratchy" throat that is followed closely by the development of nasal obstruction and rhinorrhea.
- Cough occurs in one-third of cases and frequently appears after the onset of nasal symptoms and often persists longer. The clinical features are similar in adults and children with the absence of fever in adults.
- Rhinovirus causes up to 40% of exacerbations of chronic bronchitis and is occasionally complicated by bacterial sinusitis and acute otitis media.
Diagnosis
Though clinical history and examination may give important clues toward establishing the specific viral diagnosis, they are still nonspecific. Etiologic diagnosis can only reliably be made by the detection of viruses, antigens, or nucleic acids in respiratory or other specimens or by retrospectively demonstrating an immune response in paired serum samples.
Culture
- Detection of viruses by observing the cytopathic effect and hemadsorption in cell culture has been considered the "gold standard" for diagnosis of respiratory viral pathogens for decades.
- Viruses such as adenovirus, influenza A/B, RSV, and human PIVs are the most common respiratory viruses that are isolated and detected by cell culture.
- Modified cell culture methods such as the centrifugation-enhanced shell-vial method have reduced the turnaround time from 5 to 10 days to 24 hours.
- Shell-vial culture using combination cell lines also allows simultaneous detection of multiple respiratory viruses. As compared to conventional culture, has similar sensitivity for parainfluenza 1-3 (87% vs. 83%) and influenza A/B (78% vs. 75%), and significantly higher sensitivity for RSV (73% vs. 42%).
- Notwithstanding these benefits, several viruses that are clinically significant—like coronavirus and rhinovirus—are challenging to cultivate in culture and can yield inconsistent outcomes.
Rapid antigen detection method
Most laboratories utilise one of the many readily accessible quick direct antigen detection techniques. The direct and indirect immunofluorescent assays are both sensitive (93-98%) and specific (92-97%) but require several hours and skilled laboratory personnel. Other methods available are the enzyme immunoassay (EIA) method and, to a lesser extent, the optical immunoassay (OIA), which has a sensitivity of 88-95% and specificity of 97-100% when compared with culture.
Serological tests
Serological tests are useful in detecting pathogen-specific antibodies. These antibodies typically appear about 2 weeks after initial infection and are useful in detecting most respiratory pathogens such as RSV, adenovirus, influenza A and B, and parainfluenza 1-3 viruses. However, they are still less sensitive when compared to molecular methods such as reverse transcription polymerase chain reaction (RT-PCR). They are still useful for epidemiological studies, as it increases the probability of identifying acute viral infections.
Nucleic acid amplification tests
Detection of respiratory pathogens by nucleic acid amplification tests (NAATs) such as:
- Polymerase chain reaction (PCR)
- Nucleic acid sequence-based amplification (NASBA)
- Transcription-mediated amplification (TMA)
- Strand displacement amplification (SDA)
- Loop-mediated isothermal amplification (LAMP)
- Rolling circle amplification (RCA)
It has gained immense popularity over the past decade.
Several types of specimens can be used for the detection of respiratory viruses, including:
- Bronchoalveolar lavage (BAL)
- Throat swabs
- Nasopharyngeal (NP) washes
- NP aspirates
- Lung aspirates
- NP swabs
Although the appropriate specimen type depends on the specific patient population, for optimal results, specimens should be collected within 3-5 days after the onset of symptoms to ensure a high concentration of virus particles and should be transported with an appropriate transport media at 2-8°C and testing performed within 48 hours.
Studies have reported increased diagnostic yield (60% vs. 35%) and considerably higher sensitivity (80-100%) and specificity (82-100%) for these assays when compared to conventional diagnostic methods such as direct fluorescent antibody (DFA), viral isolation, and immunoassays. Molecular testing has considerably improved the diagnosis of respiratory pathogens and is considered the new "gold standard."
Treatment
Managing viral fevers, including seasonal flu, primarily involves symptomatic relief and supportive care. This may include:
1. Rest: Ample rest allows the body to fight off the infection more effectively.
2. Hydration: Drinking fluids helps prevent dehydration, especially with fever and sweating.
3. Over-the-counter medications: Analgesics like acetaminophen or ibuprofen can alleviate fever, body aches, and headaches. Cough suppressants and decongestants may help with respiratory symptoms.
4. Antiviral medications: In some cases, antiviral drugs may be prescribed, particularly for severe or high-risk individuals, to reduce the duration and severity of symptoms
Despite the varied presentation and severity of illness following viral infections, the treatment options are mainly supportive. Antiviral agents are available for selected viruses and are recommended only in specific populations.
- Cidofovir is available for severe adenovirus infections and should be administered with probenecid simultaneously.
- Ribavirin is available as oral or aerosolised formulations for the treatment of RSV infections; however, its use is not routinely recommended except in selected patients such as extremely preterm, neonates with underlying heart or lung disease. Humanised anti-RSV immunoglobulins (palivizumab) are available for the prevention of RSV infection in these high-risk groups.
- Neuraminidase inhibitors such as oseltamivir and zanamivir, which inhibit influenza virus neuraminidase, are effective for the treatment and prophylaxis of influenza. Treatment for simple influenza is usually not necessary, but if it is, neuraminidase inhibitors must be administered within 48 hours after the onset of symptoms in order to have any therapeutic benefit.
- Treatment should not be stopped in cases of severe influenza, influenza in immunocompromised individuals, or avian influenza as benefits can still be obtained when given after 48 hours. Amantadine and rimantadine have become obsolete due to the development of resistance.
- Several drugs have been studied for SARS-CoV-2 following the epidemic. Antiviral agents such as remdesivir, antibody-based therapies such as casirivimab and imdevimab, glucocorticoids, drugs like tocilizumab and baricitinib, and anticoagulants are found to be effective depending upon the time of onset and severity of the disease.
Indian perspective
Various studies have been done to look at the prevalence of viruses causing respiratory infections in India.
- In a recent study among adults with acute respiratory infection (ARI), influenza accounted for the maximum number of cases (27.6%) followed by RSV (5.2%), hMPV (3.7%), and parainfluenza-j virus (3%).
- Earlier studies have shown a similar pattern with influenza A being predominant (17%) followed by influenza B (6.5%), RSV (5.2%), and HMPV (3.7%).
- Among children with ARI, a recent study reported RSV (25.8%) as the predominant virus followed by rhinovirus (21.9%), influenza (21%), and adenovirus (12.5%).
The study results have been similar in comparison with the past, where RSV and influenza A reported more commonly followed by parainfluenza and metapneumovirus in variable proportions.
Prevention from seasonal flu
Preventing seasonal flu and other viral fevers involves various strategies, including:
Getting vaccinated against seasonal flu is the single best way to lower your risk of contracting the illness and any potentially dangerous complications, but you can also prevent respiratory illnesses like flu by avoiding sick people, covering your cough, and washing your hands. This may also involve implementing measures for improved air quality and maintaining hygiene by regularly cleaning commonly touched surfaces. Antiviral medications are another option for treating and preventing flu.
Seasonally appropriate immunisations guard against the three flu viruses that, according to research, are most likely to be prevalent in the coming flu season.
You can learn about steps you can take to prevent the transmission of germs and safeguard yourself and others against the flu by using the tools and advice listed below.
1. Avoid close contact
Avoid close contact with people who are sick. Keep your distance from other people when you're unwell to prevent them from getting sick as well. Keeping a physical distance from other people can help reduce the chance of respiratory virus transmission.
2. Stay home when you are sick
When you're sick, try to avoid going to work, school, or doing errands. When both of these conditions are met for a minimum of 24 hours, you can resume your regular activities:
- Your symptoms are getting better overall, and
- You don't have a temperature (and you're not taking any medicine that lowers fever).
There are further safety measures that can be used to shield individuals from respiratory infections once these two requirements have been satisfied.
3. Cover your mouth and nose
- Cover your mouth and nose when coughing or sneezing. It might keep the people close to you healthy.
- People who have the flu are thought to mostly transmit the virus by coughing, sneezing, or talking. Another preventive tactic you can use to better safeguard both yourself and other people is wearing a mask.
- Masks stop the virus from spreading to other people when they are worn by the infected person. Additionally, masks help shield wearers from inhaling infectious particles from nearby individuals.
4. Clean your hands
Frequent hand washing can help keep you safer from infections. Use an alcohol-based hand rub in the absence of soap and water.
5. Avoid touching your eyes, nose or mouth
When someone touches anything contaminated with germs and then touches their mouth, nose, or eyes, they can spread those germs to other people.
6. Take steps for cleaner air
By gathering outside, purifying inside air, or bringing in fresh outside air, you can increase the quality of the air. The chance of contracting a virus can be decreased by cleaner air.
7. Practice good hygiene and other healthy habits
It can help stop the transmission of some infections by cleaning frequently touched surfaces like doorknobs, handrails, and worktops on a regular basis. In addition, make sure you get enough rest, exercise, control your stress, stay hydrated, and consume a balanced diet.
Nonpharmaceutical Interventions (NPIs)
Nonpharmaceutical interventions (NPIs) are steps that individuals and communities can do to assist in reducing the spread of diseases like the flu, aside from receiving a vaccination or taking medication.
Preventing flu at work and school
At school
- Find out what steps your child's school, daycare, and/or college will take in the event of a flu or other sickness outbreak, as well as whether on-site flu vaccinations are available.
- Find out if the school, daycare centre, or college where your child attends cleans frequently handled objects and surfaces on a regular basis and if they have an adequate quantity of tissues, soap, paper towels, alcohol-based hand rubs, disposable wipes on-site and other supplies.
- Inquire about any actions taken by your child's college, daycare centre, or school on cleaner air policies.
- Ask how sick students and staff are separated from others who will care for them until they can go home, and about the absentee policy for sick students and staff.
At work
- Find out if flu shots are provided on-site and what your company will do in the event of an illness or flu outbreak.
- Routinely clean frequently touched objects and surfaces, including doorknobs, keyboards, and phones, to help remove germs.
- Ensure that there are enough tissues, soap, paper towels, alcohol-based hand rubs, and disposable wipes available at your place of business.
- Teach people how to perform your duties so they can step in for you in the event that you or a family member becomes ill and has to stay at home.
- Leave the office as soon as you feel ill if you are at work.
In conclusion, while viral fevers like seasonal flu pose significant health challenges, understanding their causes, signs, and symptoms is essential for effective management and prevention. By adopting appropriate preventive measures and seeking prompt medical attention, when necessary, individuals can reduce the impact of viral fevers on their health and well-being.
Take home message
- Viruses are the major cause of respiratory infections.
- Influenza and RSV cause significant illness among young children and the elderly. Rapid antigen detection tests and NAATs are useful in the diagnosis.
- Vaccines against specific viruses are helpful in prevention and antiviral drugs are available for selected viruses in selected situations.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Khemeswar Agasti is an MD in General Medicine from Cuttack.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries