Comprehensive Management of Vesicovaginal Fistula
M3 India Newsdesk Oct 30, 2024
This article covers Vesico Vaginal fistula (VVF), including conservative and surgical methods. It emphasises the need for individualised care to address both physical and psychological impacts on affected women.
Vesicovaginal fistula (VVF) is defined as an abnormal connection between the bladder and the vagina. It affects the women physically, economically, psychologically and emotionally.
The most common cause of VVF in developing countries is prolonged obstructed labour whereas in developed countries pelvic surgeries are the leading cause. Poor socioeconomic status, early marriage, malnourishment, low literacy rates, and poor healthcare systems contribute to the higher prevalence of VVF in developing countries.[1]
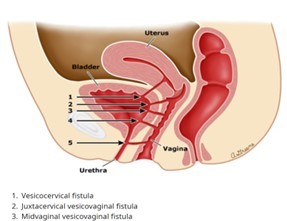
VVF, mainly obstetric, is often classified by:

Work up
History
- Examination – per speculum – tissue mobility, inflammation, infection, accessibility
- The diagnosis of a urogenital fistula is made on physical examination by visualisation of leakage of urine into the vagina or by dye test.
- Cystourethroscopy – site, size, number, b/l orifice
- IVU or CT Urography– suspicion of upper tract involvement
- RGP (negative imaging)
- Urine C/S
Management of vesicovaginal fistula
Conservative methods
Continuous bladder drainage and administration of anticholinergics have been practised with varied success rates. Percutaneous nephrostomy (PCN), PCN with bilateral ureteric occlusion, isobutyl-2cyanoacrylate injection, balloons (detachable or nondetachable), nylon plugs, coils, gelatin sponges, and fulguration are other methods for conservative treatment.
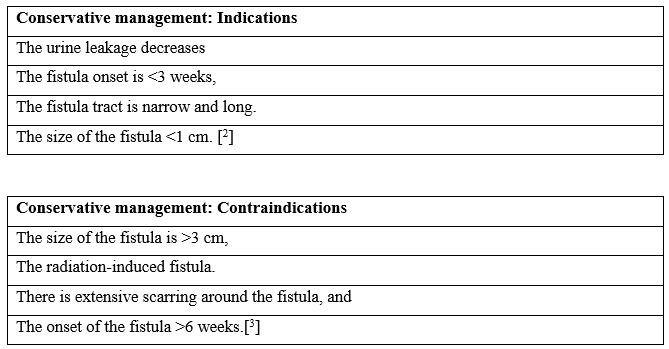
The overall success rate of CBD alone ranges between 3%–32% and if the fistula is <5 mm and there is no leakage after catheter placement, the chance of healing with CBD is high.[4]
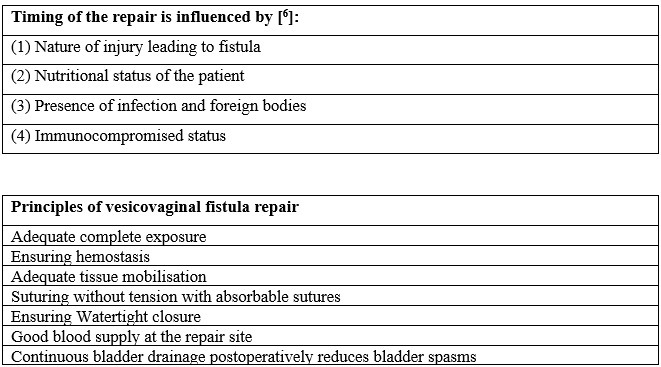
The principles of repair
Repair of the VVF is to be done when there is no active inflammation, infection, or necrosis, but repair done as soon as the VVF is diagnosed also has similar results.[5]. The highest probability of VVF repair is during the first surgery.
Route of repair-transabdominal versus transvaginal

Role of colpocleisis
Types of colpocleisis in VVF repair:
- Simon colpocleisis (transverse closure)
- Latzko colpocleisis (sagittal closure)
Latzko technique has prerequisites,[9] namely
- Post hysterectomy status
- Adequate preoperative vaginal vault length
- Proximity of the fistula to the vaginal vault
Latzko's procedure is simple with a high success rate, low morbidity and no impairment in bladder capacity or ureteral orifices. The success rate in patients with simple post-hysterectomy VVFs is 93% - 100%.[10]
Modifications in transabdominal repair
O’Connor and Sokol described the abdominal VVF repair by bivalve the bladder.[11]. Newer and recent techniques include limited vertical cystotomy,[12] horizontal cystotomy,[13] and intravesical repair [14] of VVF.
These techniques have:
- Less operating time
- Improved laparoscopic suturing and better luminal delineation,
- Less incidence of overactive bladder, and
- Early anterior dissection to reduce the tension on the suture line [13]
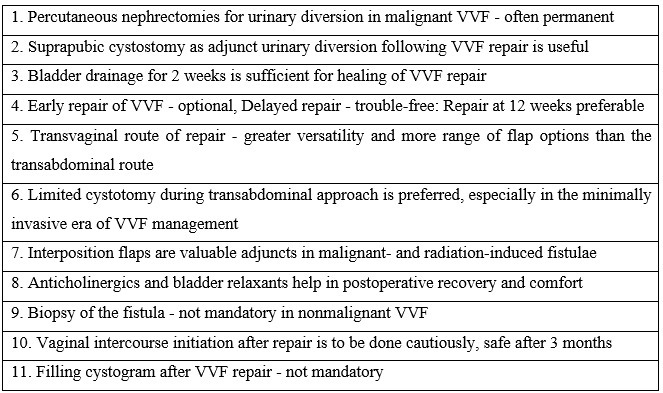
Urinary diversion after repair
To accelerate the healing process after VVF repair diversion of the urine is helpful as it keeps the suture line dry. Per-urethral catheterisation or Suprapubic cystostomy (SPC) and the duration of urinary drainage after the repair are debatable. Usually, the catheter is removed by the 14th day,[15] but may be kept longer depending on the number, size, nature of the fistula, and effectiveness of the repair.
1. Radiation-induced vesicovaginal fistula
- Pelvic radiation is the primary cause of delayed VVF.[16] The majority of the fistulae form 1.5–2 years after the completion of radiotherapy. Recurrence of malignant disease at the edges of the fistula must be excluded by multiple focal biopsies.[17]
- Complete excision of the scar till the fresh tissue margin is necessary but because of the large size a primary closure of the defect becomes difficult.
- Tissue interposition should be considered whenever the closure lines or the vaginal tissues are of questionable quality.[17] Adjacent muscle flaps have a better success rate than bulbocavernosus flaps, as the vascularity of bulbocavernosus muscle may be compromised by the previous radiation.[18]
2. Urinary diversion in inoperable vesicovaginal fistula
Urinary incontinence despite successful fistula closure may result from small bladder capacity due to the loss of tissues at the time of injury, from complete absence of the urethra or impaired urethral function.
3. Management of overactive bladder after repair
Overactive bladder (acute spasmodic pain arising from the bladder) during the postoperative period can occur despite postoperative analgesia. The highest incidence of bladder spasms was observed among patients with vault fistula, followed by those with vesicouterine fistula.[19].
4. Biopsy/excision of the fistulous tract
Biopsy is recommended when:
- History of genitourinary malignancies
- Staging for locally advanced malignancies involving the urinary bladder[20]
5. Stress urinary incontinence (SUI) after repair
- SUI can occur after VVF repair due to ischemic or iatrogenic injury to the supports of the urethra. The placement of a mid-urethral sling during the primary repair of VVF is debatable.
- Rectus fascial sling, pubococcygeal sling, plication of pubo-cervical fascia, and avoiding tight closure of the vagina with judicious use of skin grafts and Martius flaps are measures recommended to prevent SUI.[3]
7. Sexual outcomes after repair
- Evaluated 91 patients undergoing VVF repair and reported, that the sexual function in the 64 sexually active patients was significantly improved.[21].
- Found that the vaginal length decreased on average by 5 mm following surgery and larger-sized fistulas (>3 cm diameter) and reduced vaginal calibre were associated with a higher risk of postoperative sexual dysfunction.[21].
- Intercourse is prohibited for 3–6 months following VVF repair but recent studies have shown that sexual activities can be resumed as early as 6 weeks.[22]
8. Role of filling cystogram before catheter removal
There is no recommendation on timing to perform a cystogram after VVF repair. To avoid inadvertent complications, a cystogram should be performed under dynamic fluoroscopy.[23]
Conclusions
Conservative methods should be used in selected patients. The decision to repair the VVF surgically should be taken early after considering all the factors about the fistula.
Take home messages [24]
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
The author of this article: Dr Supriya Chaubey is an Assistant Professor at HIMSR, New Delhi
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries