Pelvic-Ureteric Junction [PUJ] Obstruction in Children
M3 India Newsdesk Jul 12, 2024
This article discusses the causes, diagnosis, and treatment of urinary tract infections (UTIs) in children, focusing on structural urological abnormalities like PUJ obstruction and the importance of early intervention to prevent kidney damage.
UTI in children
Infections in children often occur in the urinary tract. Infants and female children have a higher risk for urinary tract infection but present with very few signs and symptoms specific to urinary tract infection[UTI].
Infants and female children have a higher risk for urinary tract infections. However, several other underlying risk factors predispose children to UTIs. These could be urological abnormalities with a mechanical obstruction within the urinary tract such as:
- Pelvic-ureteric junction [PUJ] obstruction
- Vesicoureteric junction [VUJ] obstruction
- Posterior urethral valves [PUV]
There are other non-obstructive urological abnormalities like:
- Vesicoureteric reflux [VUR]
- Voiding dysfunction or bladder bowel dysfunction
- Bladder dyssynergia
- Hinman syndrome
- Neuropathic bladder
Recurrent urinary tract infections can lead to loss of renal function and even a single episode of UTI is sufficient to induce significant renal damage. It is important to investigate UTIs thoroughly and initiate treatment promptly.
In this review, we aim to discuss the structural urological abnormalities that lead to obstruction of urine flow and include their presentation, diagnosis, investigations and management.
Urological abnormalities
Underlying urological abnormalities are detected in almost a third of the children presenting with UTI. Non-invasive ultrasound scan [USS] imaging is the first line of radiological investigation commonly used in children.
Although ultrasound imaging is observer-dependent, it can provide valuable details on renal architecture, cortical thickness, size of renal pelvis, and bladder volume and thickness.
Further imaging studies like Micturating cystourethrogram [MCUG], Dimercaptosuccinic acid [DMSA] and Diethylenetriamine Pentaacetic Acid renal scan[DTPA] and Mercapto-acetyl tri glycine [MAG3] scans help us in the diagnosis and assessment of urological abnormalities.
Interpreting the results of imaging studies and clinical findings will determine further management, surgical intervention and follow-up in children with UTIs.
The NICE guidelines developed in the UK for UTI in children aim to address the importance of accurate diagnosis and effective subsequent investigations and treatment. Although these guidelines are robust and evidence-based, individual patient characteristics and presentations may vary and warrant further investigations and appropriate management.
PUJ (Pelvi-ureteric junction) obstruction
The most frequent cause of upper urinary tract obstruction in children is a congenital pelvic-ureteric junction (PUJ) obstruction. With the advancement of fetal ultrasonography, the majority of PUJ obstruction in children is diagnosed antenatally.
Fetal upper urinary tract abnormalities are seen in almost 1 in 100 pregnancies and pelvi-calyceal dilatation is the most common abnormality detected. The majority of these antenatally detected hydronephrosis resolve spontaneously and only 1 in 5 is later diagnosed with urinary tract problems.
Incidence
PUJ obstruction is the most common cause of neonatal and antenatal hydronephrosis, occurring in 1 per 1500 live births. However neonatal and antenatal hydronephrosis can also be seen in VUR and lower urinary tract obstruction as well. The male-to-female ratio of PUJ obstruction is 3-4:1. In general, the left kidney is more commonly affected than the right kidney.
Aetiology
Koff described two types of PUJ obstruction: Intrinsic and Extrinsic.
- In the Intrinsic type classically known as the “adynamic” segment, defective peristalsis of urine at the level of PUJ leads to obstruction and hydronephrosis.
- PUJ obstruction in the extrinsic type has been reported to be caused by mechanical causes such as sticky bands, crossing arteries, arterio-venous malformations, and fetal folds.
- Very rarely trauma and renal structural abnormalities like horseshoe kidney; and malrotation of kidneys can present with PUJ obstruction. Intraluminal stones can also cause PUJ obstruction in children.
Diagnosis
- Renal ultrasonography is the first line and non-invasive investigation for PUJ obstruction. Renal pelvis anteroposterior diameter [APD] can be measured with ultrasound and compared with standard values for children of the same age to suggest renal pelvic dilatation.
- However, the hydration of the patient along with bladder volumes has to be taken into consideration before interpreting the renal pelvic dilatation detected by ultrasound.
- The Society of Fetal Urology [SFU] has classified hydronephrosis based on the renal pelvicalyceal dilatation into 5 grades – 0 to 4. The severity of hydronephrosis increases with grade [Table]. However, a study has shown that neither the renal APD nor the SFU grading is the standard in determining the severity of antenatally detected hydronephrosis.
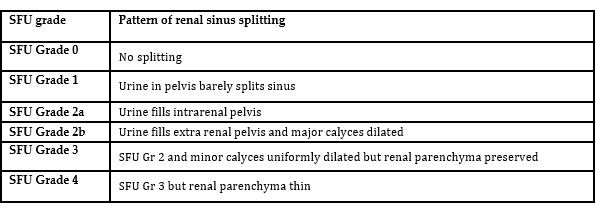
Table: Society for Fetal Urology, grading of hydronephrosis
- Traditionally, an intravenous pyelogram [IVP] has been used to diagnose PUJ obstruction. This involves injection of iodine-based contrast/dye into a superficial vein and x-ray imaging of the kidneys and urinary tract at various intervals.
- The kidneys uptake the contrast and excrete them in the urine which details and outlines the urinary tract, particularly the renal pelvis, PUJ and ureter. However, nuclear imaging has now replaced IVP and MAG3 scan is the investigation of choice. MAG3 scans provide detailed information on the drainage patterns of individual kidneys along with the differential function of each kidney.
- Administration of Furosemide [Diuretic] can reveal valuable information on further drainage patterns of kidneys. Poor drainage or no drainage suggests obstruction of the urinary tract which is most likely at PUJ in the absence of dilated ureters.
- Although MAG3 scans can give valuable information on the drainage patterns of kidneys, the evaluation of ureteral anatomy is difficult with nuclear imaging. IVP can reveal detailed anatomy of the ureter and PUJ. Retrograde injection of contrast/dye via bladder catheterisation can also reveal valuable information on the anatomy of the ureter and PUJ.
- CT scan with contrast and MR renogram and angiogram are also used that can reveal much more detail along with the diagnosis of crossing vessels obstructing the PUJ as commonly seen in older children and adults.
Role of UTI in PUJ Obstruction
- The majority of the children detected with PUJ obstruction remain asymptomatic. However, a significant number of PUJ obstructions are detected following presentation with UTI.
- Systemic infection or UTI reaching the renal pelvis and kidney can result in pyelonephritis and pyonephrosis [Pus in the renal pelvis].
- Typically the child presents with high-grade swinging pyrexia, poor feeding or vomiting and tenderloins. Serum inflammatory markers are raised; however, the serum creatinine remains stable as the contralateral kidney compensates for the loss of renal function on the ipsilateral side.
- Ultrasound scanning reveals pus and debris in the dilated renal pelvis.
- Pyonephrosis can result in significant irreversible renal damage very quickly and therefore prompt drainage is advised. Fluid resuscitation and Intravenous antibiotics should be commenced immediately.
- A nephrostomy drain is usually inserted to drain the pyonephrosis and the collecting urine under radiological guidance.
- Cystoscopy and ureteric stent insertion is an alternative to nephrostomy. Subsequent ultrasound imaging and clinical pictures determine the duration of the drain/stent left in situ. Further imaging with DMSA and MAG3 scans helps in identifying the renal damage and the severity of obstruction.
Anderson and Hynes first popularised the technique of pyeloplasty and it still remains the gold standard operation for the correction of PUJ obstruction. The success rates are pretty good around 95% or above for open surgery and recently laparoscopic approach has gained popularity with equivalent success rates. The approach is chosen by the surgeon, based on his skills/expertise, the age of the patient, co-morbidities and anaesthetic risks.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Sivasankar Jayakumar is MBBS, MRCS, FEBPS, Department of Paediatric Surgery & Urology, Apollo Cradle & Children’s Hospital, Karapakkam, Chennai.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries