Understanding the Basics of Irritable Bowel Syndrome
M3 India Newsdesk Nov 11, 2022
Irritable Bowel Syndrome (IBS) is a functional disorder of the gastrointestinal tract which leads to a cycle of chronic and unpredictable symptoms. The prevalence, prognosis, and management of IBS are covered by the author in this article.
Irritable Bowel Syndrome IBS does do not cause any physiological changes to the structure of the GI tract but rather there is some functional change happening at the bowel muscular level in the tract. This can cause some major bowel disturbances and bouts of pain.
Types of IBS
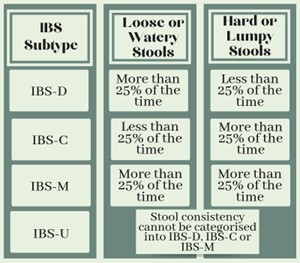
IBS is divided into three categories based on the occurrence of constipation or diarrhoea:
- IBS with constipation (IBS-C): The bowel movements are affected by constipation leading to hard lumpy stools.
- IBS with diarrhoea (IBS-D): The bowel movements are affected by diarrhoea leading to watery and loose stools.
- IBS with mixed bowel habits (IBS-M): The bowel movements are occasionally affected by both of the above.
- IBS with irregular stool consistency (IBS-U): The bowel movements cannot be categorised into any of the above categories.
Prevalence
The onset of IBS is between the late teens to twenties which gradually decreases as age increases. A few studies show that females are more predisposed to develop IBS as compared to males.
This condition can be a debilitating one based on the intensity of the symptoms and reports have shown that this affects around 9%-23% of the world population according to the World Gastroenterology Organisation, (2009) but only 12% of the population seeks help and treatment for the condition in their primary health centres.
Most of the time there is less awareness among the people about the condition which can lead to a delayed diagnosis by the doctors and also a delay in further treatment.
Pathophysiology
Past literature has explained IBS is caused because of visceral hypersensitivity and which can cause some motor disturbances leading to gastric issues like constipation and diarrhoea.
But these changes caused in gastric motility did not provide sufficient evidence in the case of the IBS-M type. It was then proposed that these disturbances could be secondary to psychological issues but then again there were many cases of IBS were reported where patients has no reports of psychological disturbances.
As these theories were neither completely accepted nor discarded. literature has proposed a few more concepts explaining the pathophysiology of IBS.
Infection-induced IBS and immune activation
There is increasing evidence of IBS related to an infection-induced condition and about 1 in 10 patients have complained of IBS-like symptoms after being affected by a GI infection. The prolonged duration of the initial illness, the toxicity of infecting bacterial strains, and mucosal markers of inflammation can be a few reasons.
Exposure to intestinal infection can lead to persistent low-grade systemic and mucosal inflammation, which is characterised by an altered population of circulating cells and mucosal infiltration of immune cells with increased production of cytokines which can lead to an exacerbation of symptoms of IBS. A few more studies have presented evidence of finding immune system activation through the release of various cells and markers in cases of patients suffering from IBS.
Central dysregulation and Impaired brain-gut interaction
Very interesting findings have been recorded in a few studies which show some significant and remarkable changes in MRI brain done for patients suffering from IBS.
There were changes observed in the cortical function in response to gut stimulation. A few changes observed showed that measures of regional cerebral blood flow during rectal distention in IBS patients have greater activation of the anterior cingulate cortex, amygdala and dorsomedial frontal cortex in contrast to healthy controls.
Serotonin dysregulation
Serotonin (5-HT)(5-HT3 and 5-HT4 receptors), plays a big role in the control of gastrointestinal motility, sensation, and secretion. It is also observed that plasma 5-HT concentrations were reduced in IBS patients with constipation but raised in those with diarrhoea. These findings support the motor and sensory dysfunction involvement associated with this condition.
Risk factors of IBS
A few risk factors that can predispose an individual to develop IBS are as follows:
- Unknown food intolerance
- Severe allergies to certain food
- Emotional stress
- Anxiety
- Family history of IBS
- Severe intestinal infections
- History of abuse
- Sleep disorders
Causes and triggers of IBS
- Unknown Dietary allergies or sensitivity towards certain foods can be a very important cause triggering IBS.
- Food that usually causes bloating or flatulence like beans, bananas, apricots or some bread products like milk items, candies, caffeinated products etc can also trigger a few symptoms.
- People suffering from mental health disorders like anxiety, depression or post-traumatic stress disorder usually show symptoms of IBS.
- A few genetic factors can also act as triggers for IBS.
- Abnormal response to a medication.
- Some hormonal imbalances.
- Menstrual cycle in the case of women.
Diagnosis
The Rome III criteria.was developed by the Rome Foundation Board and this criteria presents a standardised self-reported questionnaire, which has been used to identify Functional Gastrointestinal disorders (FGIDs).
The clinical diagnostic criteria define IBS as recurrent abdominal pain or discomfort for at least 3 days/month during the last 3 months associated with at least two or more of the following features:
- Improvement after defecation
- Onset associated with a change in frequency of bowel movement and/or
- onset associated with a change in the form (appearance) of stools
Signs and Symptoms of IBS
- Abdominal pain or cramps more towards the lower section of the abdomen.
- Irregularised bowel movements with either bout of constipation or at times diarrhoea.
- Feeling of bowel not being empty properly even after passing stools.
- Bloating and excessive flatulence.
- Mucous in stools.

Location of pain in IBS
-
Upper abdominal pain-Occurs in episodes of bloating and worsens after food intake
- Middle abdominal pain-Cramping around the belly button region
- Lower abdominal pain-Pain eases out on bowel movements
Severity and frequency of the pain in IBS
- The quality of pain is mild and nagging and in a few episodes can be severe and crippling kind of a pain.
- The frequency of pain usually follows a spurt pattern where the patient may have pain-free days with spurts and episodes of severe pain.
Differential diagnosis
A few other medical conditions can also present with similar symptoms and hence it is important to identify the correct diagnosis to provide the ideal and correct treatment
- Inflammatory bowel disorder
- Crohn’s disease
- Ulcerative colitis
- Colon cancer
- Celiac disease
- Lactose intolerance
Prognosis of IBS
Usually, IBS tends to last for a lifetime but patients do have symptom-free periods of all advisory measures followed u and sudden flareups if something is triggered. But IBS does not affect the lifespan of an individual or does not lead to any life-threatening condition.
Treatment
Dietary protocols
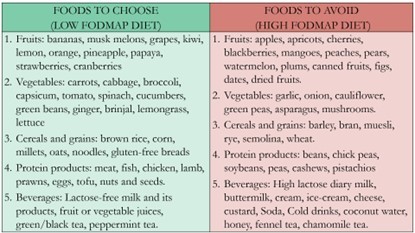
Food is a powerful tool to utilise in the management of IBS. Avoiding foods that can trigger symptoms and designing a regimen based on that can be considered as a very important and first guiding step in planning the treatment for an IBS patient
Food products to avoid in IBS:
- Highly fatty foods
- Gluten-containing products
- Food products that cause bloating or gas
- Caffeinated products or beverages
- In a few cases lactose-containing products
Food products recommended by IBS
- High dietary fibre
- Simple carbohydrates
- Easily digestible proteins like eggs, fish, tofu etc
- Gluten-free food item
- Probiotics like yoghurts
Pharmacological treatment modalities for treating IBS
If the symptoms are moderate to severe one can prescribe a combination of the following medications with the right duration and dosage in time
- Laxatives
- Anti-diarrhoea medications such as loperamide
- Anticholinergic medications like dicyclomine
- Pain medications like pregabalin or gabapentin in case of severe pain and discomfort
- Tricyclic or SSRI antidepressants in severe cases
In a few cases, some psychological tools like Cognitive behavioural therapy (CBT) and hypnotherapy could also be used if there is some evidence of psychological overlay.
Lifestyle management tips for your patients suffering from IBS
- Regulate the water intake and have maximum fluids throughout the day.
- Switch to a short-term FODMAP diet for some time.
- Switching to more cooked food rather than raw as it makes it easy to digest.
- Include exercise in your daily routine as this can help in reducing gas and bloating.
- Limiting sugar intake.
- Keeping a check on stress and anxiety.
- Limiting alcohol intake and smoking.
- Maintaining a regular sleep pattern.
Disclaimer- The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Ridima Surve is a practising dentist from Mumbai.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries