TMJ Ankylosis: Diagnosis and Management
M3 India Newsdesk Jul 23, 2024
The Temporomandibular Joint (TMJ) is a specialised joint that can be classified by anatomic type as well as by function. This article explains what is TMJ ankylosis, its pathogenesis and its management.
TMJ ankylosis
The temporomandibular Joint (TMJ) is a complex structure composed of several components including the glenoid fossa of the temporal bone, the condylar head of the mandible & a specialised dense fibrous connective tissue structure of the articular disk as well as several ligaments & associated muscles.
Ankylosis is a Greek word that means a “stiff joint”
It refers to partial or whole incapacity to open the mouth, leading to abnormalities in the mandible's growth or function. Ankylosis can cause anything from a straightforward fibrous restriction of jaw mobility to a bone development inside the joint that totally restricts movement.
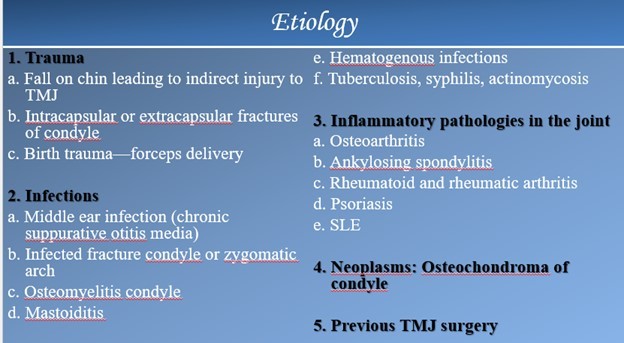
Aetiology
Pathogenesis for ankylosis
Intra-Articular Hematoma as the Principal Cause of Ankylosis: The TMJ's organisation and subsequent ossification support the theory that intra-articular hematomas alone may cause ankylosis. Since this theory is based on experimental research, it might not match what is observed in vivo.
Nevertheless, there is a theory that contradicts this one: because traumatic haemorrhage in the joint area does not necessarily result in the formation of bone, it may not produce ankylosis.
Classification
According to Topazian
- Stage 1: Ankylotic bone confined to the condylar mechanism
- Stage II: Ankylotic bone limited to the sigmoid notch
- Stage III: Ankylotic bone limited to the coronoid process
According to Sawhney
- Type I: Minimum bony fusion but extensive fibrous adhesion
- Type II: Bony fusion at the outer edge of the articular surface but no fusion on the medial area
- Type III: Bridge of bone between the mandible & temporal bone
- Type IV: Joint replaced by a mass of bone
Diagnosis
History
- Accurate history is important to differentiate the conditions of pseudo ankylosis & true ankylosis.
- History of trauma, either to the chin directly or indirectly through the joint.
- The duration of the trismus should be asked.
- It is important to rule out extracapsular causes, such as an untreated zygomatic arch fracture.
- History of ear infection in childhood.
- History of forceps delivery of the child.
Clinical examination
Restricted mouth opening, the patient will complain of difficulty in mastication. Protrusive movements are absent on the involved side. Palpation reveals either partial or total immobility of the condyle.
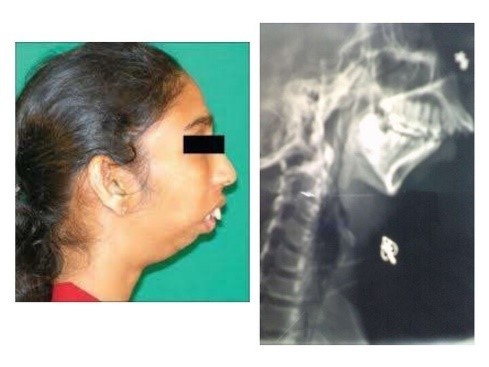
- Unilateral Ankylosis: Facial asymmetry, affected side appears normal, opposite side appears flat, chin deviated to ankylosed side, deep ante gonial notch on ankylosed side, reduced condylar movements on the affected side, class II malocclusion on the affected side, decreased mouth opening, posterior crossbite, poor oral hygiene.

- Bilateral Ankylosis: Bird face, trismus, class II malocclusion, deep antegonial notch, poor oral hygiene, crowding of teeth, protrusion of upper anterior teeth, anterior open bite, no condylar movements palpable.
Investigations
- Radiographs: Posteroanterior (PA) mandible and orthopantomogram show the distorted anatomy of ramus, condyle and coronoid process, the bony fusion between the mandibular condyle and glenoid fossa and its extent, involvement of sigmoid notch, widening and elongation of coronoid process, shortening of ramal length, accentuated antegonial notch, retruded mandible, and canting of occlusion.
- Computed Tomography Scan: Axial and coronal sections and three-dimensional reconstruction show the medial extent of ankylosis, which is not visible on the conventional radiographs
- High-Resolution Computed Tomography with Contrast Angiogram: CT angiography can be a useful adjunct in the treatment of patients with TMJ ankylosis with a large mass or recurrence or a history of several prior TMJ procedures to ascertain how the mass and medial vasculature are related. Magnetic resonance angiography provides an alternate source of vascular imaging.
Management
- Condylectomy: performed in cases of ankylosis in which the joint's anatomical characteristics are not entirely altered, as opposed to fibrous or partial ankylosis. The condylar area is exposed through the placement of an incision. The area around the condyle's neck is sliced horizontally. The condyle head is cautiously separated after being sectioned at the level of the neck. The entire head of the condyle is separated and eliminated because the superior attachment is not firmly attached. The stump of the condyle at the neck is smoothened and thus a new joint is created.
- Gap arthroplasty: This procedure creates an artificial joint space by making an anatomical gap in the ankylosed segment. Commonly done in case of complete ankylosis. A gap in the bone is created to spare the ramus from ankylosed mass in the glenoid fossa. 2 horizontal bony cuts are made in the most superior aspect of the ramus and the wedge of the bone between the 2 cuts is removed.
- Interpositional arthroplasty: When Gap Arthroplasty is done to release ankylosis, there are chances of contact between the bone ends to form a reankylosis. So interpositional material is to be placed in between them to avoid contact and minimise chances of reankylosis. Alloplastic or autogenous materials can be used.
Kaban’s protocol for the management of Temporomandibular Joint Ankylosis
- Aggressive excision of fibrous and/or bony mass
- Coronoidectomy on the affected side
- Coronoidectomy on the opposite side of steps 1 and 2 do not result in mouth opening of >35 mm or to the point of dislocation of the opposite side
- joint lining made of natural disc material or temporalis fascia, if salvageable
- Reconstruction with a costochondral graft
- Rigid fixation
- Early mobilisation of jaw (not >10 days) & Aggressive physiotherapy
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Dhyey Saradhara is a practising dentist and an oral and maxillofacial surgeon from Surat.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries