Thyroid Function in Pregnancy: Management for Maternal and Foetal Health
M3 India Newsdesk Oct 11, 2023
This article discusses how pregnancy affects thyroid function, highlighting the significance of trimester-specific reference ranges for thyroid hormones and the care of thyroid problems throughout pregnancy to protect the health of both the mother and the growing foetus.
Pregnancy is accompanied by metabolic and hormonal changes associated with the thyroid gland. It is therefore important to understand the underlying physiological alterations and the management of patients with thyroid disorders in pregnancy.
Thyroid hormone changes in pregnancy
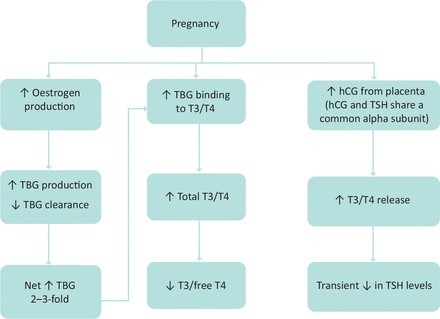
Pregnancy results in a rise in the total T4 and T3 levels due to an increase in thyroid binding globulin (TBG) levels and a reduction of TSH levels due to the thyrotrophic effect of human chorionic gonadotrophin (hCG) released from the placenta.
Therefore, there is a consensus for an adapted trimester-specific reference range for T3, T4 and TSH. The upper limit of total T4 levels in the second and third trimester of pregnancy is to be multiplied by ∼1.5 times the normal range of pre-pregnancy values.
Although the foetal thyroid gland is present and functional by 10–12 weeks of gestation, it does not mature until 18–20 weeks. Thus, the foetus depends on maternal thyroid hormone delivered via transplacental passage during a critical period of development in early gestation.
Consequently, maternal thyroid dysfunction can lead to adverse pregnancy and child neurodevelopmental outcomes. Women before pregnancy, during pregnancy and while breastfeeding should aim to increase their daily iodine intake to 250 μg.
The accuracy of serum FT4 measurement by the indirect analogue immunoassays is influenced by pregnancy and varies significantly by manufacturer. If measured in pregnant women, assay method-specific and trimester-specific pregnancy reference ranges should be applied.
Total T4 measurement is a highly reliable means of estimating hormone concentration during the last part of pregnancy. Accurate estimation of the FT4 concentration can also be done by calculating an FT4 index.
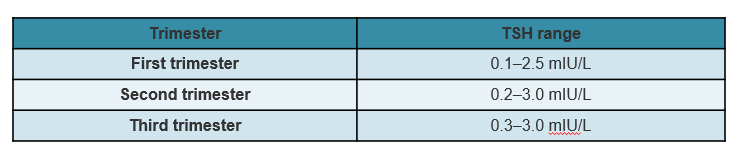
If trimester-specific reference ranges for TSH are unavailable in the local laboratory, the recommended reference ranges are available in the table.
Screening for hypothyroidism in pregnancy
Hypothyroidism in pregnancy
- Overt maternal hypothyroidism has serious deleterious effects on the foetus, like premature birth, low birth weight, miscarriage, gestational hypertension, and impaired foetal neurocognitive development.
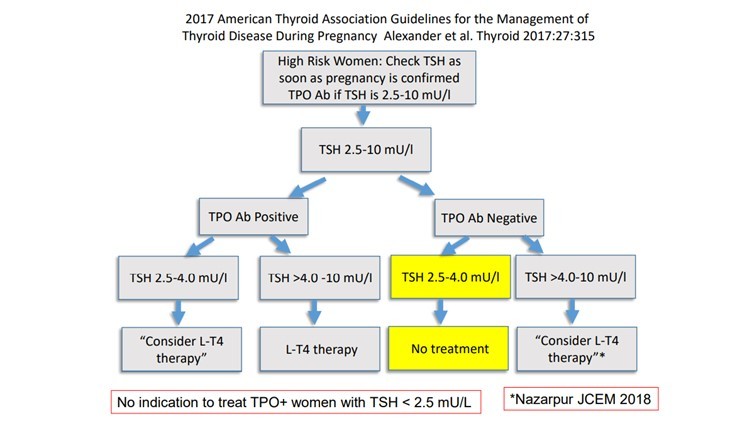
- Hypothyroidism diagnosed during pregnancy can be treated according to TSH levels. Levothyroxine dose is typically increased by approximately 30% to 50%, compared to the pre-pregnancy dose.
- Thyroid function tests (TFTs) should be performed every 4–6 weeks to ensure adequate dosing in response to the TSH levels.
- Levothyroxine is to be given in the early morning, empty stomach and do not give beverages or food for up to one hour after levothyroxine. Iron, calcium tablets and aluminium-containing antacids are to be given four hours after levothyroxine as they interfere with LT4 absorption.
Hyperthyroidism in pregnancy
- Overt hyperthyroidism in pregnancy is defined as a TSH value below the reference range of pregnancy with elevated free T4 or elevated total T4 & total T3 (1.5 times the normal range of pre-pregnancy).
- In the first trimester, especially in those with hyperemesis gravidarum and carrying twins, have suppressed TSH with elevated free T4 due to HCG, it is called Gestational transient thyrotoxicosis (GTT).
- GTT typically resolves by 18–19 weeks and it can be differentiated from Graves’ disease by the absence of TSH receptor antibodies. GTT does not need anti-thyroid medication.
- A suppressed or undetectable TSH level (<0.01 mU/l) with elevated free T4 and free T3 levels, with positive TSH receptor antibodies (TRAB), differentiates between Grave's disease and gestational transient thyrotoxicosis.
- For subclinical maternal hyperthyroidism (suppressed TSH & normal q-free T4), there is a lack of evidence that intervention with anti-thyroid medication improves pregnancy outcomes.
- In patients with overt hyperthyroidism, Propylthiouracil (PTU) is the treatment of choice in the first trimester of pregnancy as carbimazole (CBZ) is associated with congenital abnormalities, including choanal and oesophageal atresia, aplasia cutis.
- Carbimazole or methimazole is recommended from the second trimester, given the rare but severe liver toxicity associated with PTU at a conversion of 100 mg PTU to 10 mg of CBZ.
- Anti-thyroid medications should be initiated and titrated to maintain the free T4 in the upper limit of the non-pregnant reference range.
- Features suggesting foetal thyroid dysfunction may include growth restriction, hydrops, presence of foetal goitre, tachycardia, or foetal cardiac failure. Foetal anatomy ultrasound was undertaken at week 18–22 and repeated every 4–6 weeks.
- Radioactive iodine treatment is contra-indicated in pregnancy.
- Subtotal thyroidectomy may be indicated during the second trimester of pregnancy for maternal Graves' disease if serious adverse reaction to anti-thyroid drugs or a requirement of a high dose of anti-thyroid medication persistently.
Postpartum thyroiditis
Postpartum thyroiditis is the most common cause of thyrotoxicosis post-pregnancy. It typically occurs within 6 months after delivery with an initial hyperthyroid phase and then spontaneous remission thereafter.
β-blockers are the mainstay of treatment in symptomatic patients in the hyperthyroid phase.
Thyroid nodules in pregnancy
- Thyroid ultrasonography is the best imaging modality for the evaluation of thyroid nodules found in pregnant women.
- Serum levels of TSH should be checked with thyroid nodules to screen for hyperfunctioning nodules.
- A serum level of TSH that remains suppressed beyond 16 weeks gestation suggests the presence of a toxic adenoma and fine needle aspiration (FNA) biopsy can be delayed until nuclear scanning is feasible after delivery.
- If TSH is normal or elevated and the nodule meets the criteria for cytological evaluation, an FNA biopsy of the thyroid nodule can be safely performed.
- ATA recommends that most pregnant women with newly diagnosed differentiated thyroid cancer (DTC) be monitored conservatively with serial thyroid ultrasonography during pregnancy. If needed, thyroidectomy is safest in the second trimester.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Ganesh Patti MBBS, MD, DM Consultant Endocrinologist, MRCP SCE Endocrinology (UK).
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries