Thyroid Disorders and Management in Pregnancy
M3 India Newsdesk Nov 04, 2024
Hypothyroidism is one of the common endocrine disorders encountered in pregnancy. This article explains the maternal and foetal aspects of hyperthyroidism along with its management.
Hypothyroidism in pregnancy adds to the physiological stress of pregnancy. It not only affects the mother but maternal hypothyroidism has got fetal and neonatal aspects as well. [1]
The burden of hypothyroidism in pregnancy worldwide is 1.5-4 % while in India is 11%. The prevalence of hypothyroidism is 15.1 %, 12.06 %, and 14.36 % in the first, second, and third trimester, respectively. [2]
Pathophysiology
The maternal thyroid volume increases by 10-30 % during pregnancy (third trimester) due to increase in extra cellular fluid and blood volume.There are also changes in thyroid function and thyroid hormone levels in pregnancy. The total and bound thyroid hormone levels increase in pregnancy with an increase in thyroid-binding globulin (TBG).
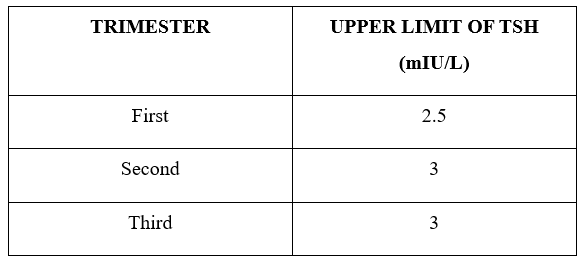
HCG shares a common alpha sub unit with TSH ,that leads to weak stimulation of TSH receptors during first 12 weeks and this increases thyroid hormone production. Increased serum free Thyroxine(T4) suppresses thyrotrophin releasing hormone(TRH) which limits TSH. After the first trimester, the TSH levels increase due to placental growth and production of placental de-iodinase.
While interpreting the results during pregnancy these physiologic changes should be remembered. [3]
Clinical features
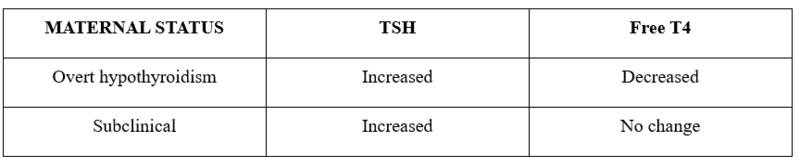
Hypothyroidism in pregnancy can present as overt hypothyroidism or sub-clinical hypothyroidism. They are distinguished by the presence of normal T4 levels in sub-clinical hypothyroidism and decreased T4 levels in overt hypothyroidism with TSH being increased in both cases.
Overt hypothyroidism complicates 2-10/1000 pregnancies and the prevalence of sub-clinical hypothyroidism is 2-5%. [3]
The clinical features of hypothyroidism overlap with those of normal pregnancy like fatigue, constipation, cold intolerance, muscle cramps and weight gain. There can be oedema, dry skin, hair loss and prolonged relaxation phase of deep tendon reflexes.
Goitre is found in cases of Hashimoto thyroiditis and those from endemic iodine-deficient areas. Hashimoto thyroiditis is the most common cause of hypothyroidism in pregnancy and is characterised by the presence of anti-thyroid peroxidase(TPO) antibodies that lead to glandular destruction.
Sub-clinical hypothyroidism doesn’t usually progress to overt hypothyroidism in healthy women. However, pregnancies with sub-clinical hypothyroidism are complicated by placental abruption and preterm births. [4]
Maternal aspects of hypothyroidism
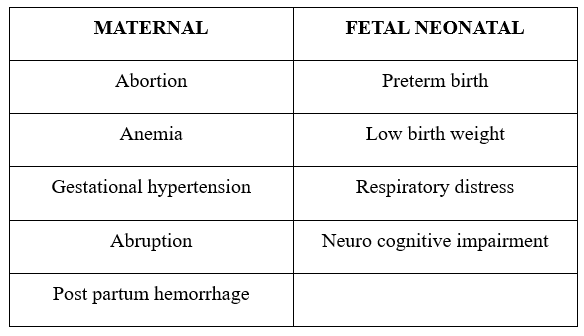
Hypothyroidism leads to decreased fertility in women. In pregnancy, it carries a greater risk of abortions, gestational hypertension, anaemia, abruption placenta and postpartum haemorrhage. In comparison, these complications are more in patients with overt hypothyroidism than in sub-clinical hypothyroidism. [5]
Foetal aspects of hypothyroidism
Overt untreated hypothyroidism leads to low birth weight babies with impaired neuropsychiatric development.
The incidence of maternal thyroid inhibitory antibodies crossing the placenta to cause fetal hypothyroidism is rare and prevalence is 1 in 1.8 lakhs neonates. [3]
There were reports of impaired neurodevelopment in offspring of sub-clinical hypothyroidism however the CATS trial (Controlled Antenatal Thyroid Screening) showed no difference in infants of mothers treated for sub-clinical hypothyroidism. The follow-up showed no neuro-developmental improvement as well. The current evidence doesn’t support the treatment of sub-clinical hypothyroidism during pregnancy for these outcomes. [3]
Management
- Universal screening is not practiced by ACOG.However FOGSI and ITS recommend routine screening for thyroid dysfunction. Venous blood samples are taken with other ANC investigations.
- The drug of choice is Levothyroxine. It is a category A drug with strength of 25,50,100 µg. It is taken orally, empty stomach with a gap of 30 minutes.
- Patients with overt hypothyroidism with TSH >2.5 mIU/L should be treated with levo -thyroxine (LT4) 1.6-2 µg /kg/day with target TSH levels being ≤ 2.5 mIU/L. Regular TSH monitoring is done every 4-6 weeks till mid-gestation and at least 28 weeks. In patients with pre-existing hypothyroidism, the dosage of LT4 is raised by 30%.
- In women of sub-clinical hypothyroidism with TSH >10 mIU/L and TSH 4-10 mIU/L with TPO Ab +ve, LT4 therapy is recommended.
- LT4 therapy can be considered in women with TSH 4-10 mIU/L with TPO Ab -ve and TSH 2.5-4 mIU/L with TPO Ab +ve.
- Post delivery the pre-pregnant LT4 dosage is to be given.Those with hypothyroidism detected during pregnancy and LT4 dose <50 µg /day can stop taking the medication. However, in both cases, TFTs should be done after 6 weeks post-delivery. Those women with anti-TPO antibodies +ve need annual monitoring of TSH.
- In postpartum thyroiditis, one of the presentations can be hypothyroidism alone or can follow hyperthyroidism. Most women recover within a year. If they are asymptomatic with mildly abnormal TFTs no treatment is needed and monitoring is to be done 4-6 weekly.
- In cases of symptomatic hypothyroidism or with TSH >10mIU/L treatment with LT4 is done(50-100 µg /day). [5]
Abbreviations
- TBG: Thyroid binding globulin
- TSH: Thyroid stimulating hormone
- TRH: Thyrotrophin-releasing hormone
- TFT: Thyroid function test
- LT4: Levo-thyroxine
- Ab: Antibodies
- +ve: Positive
- -ve: Negative
- ACOG: American College of Obstetricians and Gynecologists
- µg: micrograms
- mIU/L: Milli International units per litre
- CATS trial: Controlled Antenatal Thyroid Screening
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Nancy Jena is a PG Resident (Obstetrics & Gynaecology) from Bhubaneshwar, Odisha.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries