The MMR Vaccine: Preventing Mumps and Its Importance in Public Health
M3 India Newsdesk May 29, 2024
Explore the significance of the MMR vaccine in combating mumps outbreaks, its role in preventing complications, and the importance of maintaining herd immunity. Delve into vaccination challenges, debunked controversies, and global health equity initiatives.
Mumps outbreak
In recent weeks, in this scorching hot summer season the health authorities in different parts of India including Delhi NCR, Kerala, and Odisha reported a surge in mumps cases, a viral infection that affects mostly children and some adults.
Introduction
Mumps, once a common childhood illness, has largely been relegated to the annals of history thanks to the development and widespread use of vaccines. The MMR (measles, mumps, and rubella) vaccine stands as a cornerstone in the fight against these diseases, effectively preventing their spread and protecting public health. Among these diseases, mumps presents unique challenges due to its highly contagious nature and potential for serious complications. Understanding the importance of the MMR vaccine in preventing mumps is crucial for maintaining public health.
The threat of mumps
Mumps is a viral infection caused by the mumps virus, a paramyxovirus, a member of the Rubulavirus family. Typically characterised by swelling of the salivary glands, leading to a characteristic "hamster-like" facial appearance. While mumps is often associated with childhood, it can affect individuals of any age. The virus spreads through respiratory droplets or saliva, making it highly contagious, especially in crowded environments such as schools, colleges, and military barracks.
Mumps is most recognised for causing puffy cheeks and a tender, swollen jaw. This occurs due to the swelling of the salivary glands located under the ears on one or both sides, commonly known as parotitis.
Other symptoms that may appear a few days prior to the onset of parotitis include:
- Fever
- Headache
- Muscle aches
- Tiredness
- Loss of appetite

Symptoms typically appear 16-18 days after infection, but this period can range from 12 to 25 days. Some individuals with mumps experience only mild symptoms, similar to a cold, or have no symptoms at all, making them unaware that they have the disease. Most people with mumps recover completely within two weeks.
Although mumps are usually not life-threatening, they can lead to severe complications, including meningitis, encephalitis, deafness, and orchitis (inflammation of the testicles), which can result in infertility in males, and oophoritis in females.
Additionally, outbreaks of mumps can strain healthcare systems and disrupt normal activities, causing significant economic and social impacts.
The MMR vaccine: A shield not only against mumps
The MMR vaccine provides effective protection against mumps by stimulating the body's immune system to produce antibodies against the mumps virus. It is typically administered in two doses, the first at 12-15 months of age and the second at 4-6 years of age. In addition to mumps, the vaccine also protects against measles and rubella, two other highly contagious diseases with potentially serious complications.
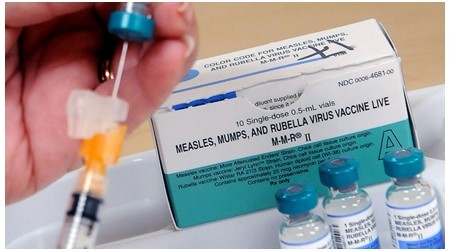
The MMR vaccine has been instrumental in reducing the incidence of mumps since its introduction in the 1960s. Prior to the vaccine, mumps epidemics were common in the United States, affecting hundreds of thousands of individuals annually. However, widespread vaccination efforts have led to a dramatic decline in mumps cases, with outbreaks becoming increasingly rare.
Who should get the MMR vaccine?
- Children
- Students at post-high school educational institutions
- Adults
Students at post-high school educational institutions & Adults who do not have presumptive evidence of immunity should get at least one dose of MMR vaccine. Certain adults may need 2 doses.
International travellers
Individuals aged 6 months and older who are planning to travel internationally should be vaccinated against measles. Prior to any international travel—
- Infants aged 6 to 11 months should receive a single dose of the MMR vaccine. Those who receive this initial dose before their first birthday should be administered two additional doses: one between 12 and 15 months of age, and another at least 28 days later.
- Children aged 12 months and older should be given two doses of the MMR vaccine, with a minimum interval of 28 days between doses.
- Teenagers and adults lacking presumptive evidence of immunity to measles should also receive two doses of the MMR vaccine, spaced at least 28 days apart.
Healthcare personnel
Healthcare personnel should possess documented proof of immunity, as recommended by the Advisory Committee on Immunisation Practices. Those without such evidence should receive two doses of the MMR vaccine, spaced at least 28 days apart.
Women of childbearing age
- Before becoming pregnant, women of childbearing age should consult their healthcare provider to confirm their vaccination status. Those who are not pregnant and lack documented evidence of immunity should receive at least one dose of the MMR vaccine.
- MMR vaccination is considered safe for breastfeeding women. Breastfeeding does not hinder the effectiveness of the MMR vaccine, and the vaccine does not pose any risk to the baby through breast milk.
Groups at heightened risk for mumps due to an outbreak of the disease
- During a mumps outbreak, public health officials may suggest an extra dose of the MMR vaccine for individuals belonging to high-risk groups for contracting mumps. These groups typically include those who are prone to close contact, such as sharing sports gear or beverages, kissing, or residing in close proximity to someone with mumps.
- Your local public health authorities or institution will notify these high-risk groups about the need for this additional dose. If you've already received two doses of MMR, there's no need to seek further vaccination unless you fall into this high-risk category.
Who should not get the MMR vaccine?
- Person with severe, life-threatening allergies.
- Pregnant women
-Pregnant women or those who suspect they might be pregnant should postpone receiving the MMR vaccine until after they have given birth. It's advised that women wait for at least one month after receiving the MMR vaccine before attempting to conceive.
- Person with a weakened immune system
-As a result of illness (like cancer, HIV/AIDS, or tuberculosis) or medical interventions (such as radiation, immunotherapy, steroids, or chemotherapy). Has a family history of immune system disorders in a parent, sibling, or relative.
- Other vaccines in the past 4 weeks.
-Administering live vaccines in close succession may result in reduced efficacy.
- Person not feeling well.
-Typically, a mild illness like a common cold doesn't usually necessitate delaying a vaccination. However, individuals who are moderately or severely ill may be advised to postpone vaccination. It's best to consult your doctor for guidance in such cases.
Challenges and controversies
Despite its proven efficacy and safety record, the MMR vaccine has faced challenges and controversies, largely fueled by misinformation and misconceptions. One such controversy arose from a now-debunked study linking the MMR vaccine to autism, which led to a decrease in vaccination rates and subsequent outbreaks of measles and mumps in various parts of the world. However, numerous studies have since refuted any association between the MMR vaccine and autism, reaffirming its safety and importance in public health.
Maintaining herd immunity
One of the key principles behind vaccination is the concept of herd immunity, which occurs when a significant portion of the population is immune to a disease, thereby providing indirect protection to those who are not immune, including individuals who cannot be vaccinated due to medical reasons. Maintaining high vaccination rates, particularly for diseases like mumps that are highly contagious, is essential for achieving and sustaining herd immunity.
The MMR (measles, mumps, and rubella) vaccine stands as a cornerstone in the field of public health for several reasons:
1. Prevention of highly contagious diseases: The MMR vaccine effectively prevents three highly contagious diseases: measles, mumps, and rubella. These diseases spread rapidly in populations with low vaccination rates, leading to outbreaks that can overwhelm healthcare systems and pose significant public health challenges.
2. Reduction of disease burden: Before the introduction of the MMR vaccine, measles, mumps, and rubella were widespread, causing significant morbidity and mortality, particularly among children. Vaccination programs have substantially reduced the incidence of these diseases, preventing countless cases, hospitalisations, and deaths.
3. Protection of vulnerable populations: Certain groups, such as infants who are too young to be vaccinated and individuals with compromised immune systems, are at higher risk of severe complications from measles, mumps, and rubella. By vaccinating the majority of the population, herd immunity is achieved, providing indirect protection to vulnerable individuals who cannot receive the vaccine themselves.
4. Prevention of complications: Measles, mumps, and rubella can lead to serious complications, including pneumonia, encephalitis, deafness, infertility, and congenital rubella syndrome (if contracted during pregnancy). The MMR vaccine significantly reduces the risk of these complications, enhancing overall public health and well-being.
5. Eradication efforts: The goal of eradicating measles, mumps, and rubella globally is within reach due to vaccination efforts. Achieving and maintaining high vaccination coverage rates is essential for eliminating these diseases and preventing their reintroduction.
6. Cost-effectiveness: Vaccination programs, including the MMR vaccine, are highly cost-effective investments in public health. The economic benefits of preventing diseases, reducing healthcare expenditures, and averting productivity losses far outweigh the costs of vaccination.
7. Global health equity: Access to the MMR vaccine and other vaccines is crucial for promoting health equity worldwide. Efforts to ensure equitable vaccine distribution, particularly in low-income countries, are essential for reducing disparities in disease burden and improving global health outcomes.
Conclusion
In conclusion, the MMR vaccine plays a pivotal role in public health by preventing measles, mumps, and rubella, reducing disease burden, protecting vulnerable populations, preventing complications, supporting eradication efforts, promoting cost-effectiveness, and advancing global health equity. By preventing mumps, the vaccine not only spares individuals from the discomfort and potential complications of the disease but also helps prevent outbreaks and their associated societal and economic costs.
Continued investment in vaccination programs and efforts to address vaccine hesitancy is essential for maximising the public health benefits of the MMR vaccine and other vaccines. Efforts to promote vaccination, combat misinformation, and ensure equitable access to vaccines are essential for maintaining the effectiveness of the MMR vaccine and safeguarding the health of communities worldwide.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Khemeswar Agasti is an MD in General Medicine from Cuttack.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries