Stepwise approach to evaluate and treat NAFLD: Prof. Dr. Ajay Duseja
M3 India Newsdesk Nov 22, 2020
NAFLD, now recognised as a multisystem disease, has the propensity to progress to liver cirrhosis and hepatocellular carcinoma. Asian‐Indians are somehow more susceptible to insulin resistance and thus to NAFLD. Treatment recommendations for NAFLD are aimed towards weight reduction, thereby reducing insulin resistance.

Nonalcoholic fatty liver disease (NAFLD) is the most common liver disease world over including countries from Asia Pacific. The global prevalence among the general population is ~25% with the highest prevalence seen in the Middle East and South America and the lowest in Africa.
The prevalence of NAFLD in general population in India varies from 9 to 53% with lower prevalence in rural areas. NAFLD is the most common cause of an asymptomatic rise in transaminases, cryptogenic cirrhosis, and cryptogenic hepatocellular carcinoma. Patients with NAFLD are also at high risk for developing type 2 diabetes mellitus, coronary artery disease, chronic kidney disease, and osteoporosis.
Severity of NAFLD may vary between individuals being effected by various factors. Hence a stepwise practical approach is important in managing patients with NAFLD.
Definition of Nonalcoholic Fatty Liver Disease
Nonalcoholic fatty liver disease (NAFLD) has been defined as the accumulation of fat in the liver in the absence of recent or ongoing intake of significant amount of alcohol and the exclusion of other secondary causes of hepatic steatosis.
Even though it is best defined by histology, accumulation of fat in the liver (fatty liver) is usually diagnosed on ultrasound (abdomen) as the liver appearing hyperechogenic in comparison to the renal cortex. The severity of fatty liver on ultrasound is graded as mild, moderate and severe based on the liver echogenicity, loss of echoes from walls of the intrahepatic portal venous radicles and posterior beam attenuation with blurring of the diaphragm.
Even though the ultrasound is a good modality to assess the presence and severity of fat in the liver, it may not be good modality to assess the overall severity of liver disease in patients with NAFLD. The criteria for the diagnosis of fatty liver on other imaging techniques like CT scan and MRI of abdomen are different from that seen on ultrasound.
Spectrum of NAFLD
Non-alcoholic fatty liver disease is a broad term consisting of patients with nonalcoholic fatty liver (NAFL) or simple steatosis, nonalcoholic steatohepatitis (NASH) which has the propensity to progress on to NASH-related cirrhosis, and NASH-related hepatocellular carcinoma (HCC).
The differentiation between NAFL and NASH is very important in determining the prognosis, risk of progression, treatment stratification and for assessing the liver-related and cardiovascular morbidity and mortality, occurring more commonly in patients with NASH than in those with NAFL.
Patients with NAFL have hepatic steatosis without hepatic inflammation or fibrosis. NASH is usually a histological diagnosis and is defined as steatosis associated with the presence of inflammation (lobular inflammation) and features of hepatocyte injury like ballooning of hepatocytes and Mallory hyaline with or without associated hepatic fibrosis. Hepatic fibrosis can be predicted or diagnosed with the help of non-invasive parameters including the use of transient elastography (Fibroscan) or other forms of hepatic elastography if available.
Evaluation of adult patients after detection of fatty liver (with or without symptoms)
Step 1: History of alcohol intake
- Alcohol intake yes– Quantify significant intake as >20g/day or >140g/week for men and >10g/day or >70g/week for women (approximately 30 ml of whisky/spirit = 100 ml of wine = 240 ml of beer = 10 g of alcohol)
- If abstainer or insignificant intake- categorise as nonalcoholic
Step 2: If nonalcoholic, assess for the presence or absence of metabolic syndrome
Metabolic syndrome is a clinical syndrome characterised by the constellation of various components namely, obesity, type 2 diabetes, dyslipidaemia, and hypertension and is usually defined by the presence of at least 3 of the following 5 components as per the WHO criteria
- Central obesity
- Waist circumference ³ 90 cm in males and ³ 80 cm in females for Asians
- Population specific cut offs for other populations
- Diabetes mellitus on treatment or fasting plasma glucose (FPG) of ³ 100 mg/dl
- Hypertension (BP ³ 130/85 mm Hg)
- Low serum HDL(<40 mg/dl or 1.0 mmol/L in males and <50 mg/dl or 1.3mmol/L in females)
- High serum triglycerides (³ 150 mg/dl or 1.7 mmol/L)) or on treatment
Step 3: If metabolic syndrome or any of its components are present
Fatty liver is likely to be nonalcoholic fatty liver disease (NAFLD)
Step 4: If metabolic syndrome or any of its components are absent
Search for other causes of hepatic steatosis other than alcohol use including history of drugs causing hepatic steatosis like corticosteroids, methotrexate, tamoxifen, amiodarone etc. and hepatitis C virus infection by anti HCV testing. Other secondary causes of fatty liver like Wilson’s disease, abetalipoproteinaemia, lipodystrophy and parentral nutrition are uncommon and may require exclusion in appropriate setting.
Step 5: Assessment of liver function tests (LFTs)
- Serum bilirubin is usually normal unless patient has progressed on to cirrhosis or HCC
- ALT may be normal or elevated
Step 6: Evaluate for other causes of raised transaminases if present
All patients with raised ALT (>1.5 times the normal) should be tested for hepatitis B surface antigen (HBsAg) and antibodies to hepatitis C virus (anti-HCV). Depending upon the clinical context, patients may also require further work-up including autoimmune markers, celiac disease work-up, serum iron profile, and serum ceruloplasmin. The presence of raised transaminases is insufficient to distinguish between NAFL and NASH.
Step 7: Non-invasive assessment for the severity of liver disease (Irrespective of elevation of transaminases)
Non-invasive assessment for disease severity and hepatic fibrosis should be done by:
- AST/ALT ratio, AST to platelet ratio index (APRI), NAFLD fibrosis score (NFS) or by transient elastography (Fibroscan) or other forms of hepatic elastography if available. Calculation of APRI and NFS is simple and can be done using free online calculators with age, BMI, diabetic status and lab parameters like AST, ALT, albumin and platelets.
- Patients with AST/ALT ratio > 1, APRI > 0.7, NFS > 0.675 and liver stiffness measurement (LSM) on ≥ 8 kPa on Fibroscan are categorised as having significant fibrosis.
- Diagnosis of NASH related cirrhosis liver and HCC may be suspected clinically or on imaging as per the clinical presentation of the patient.
- Diagnosis of NASH related cirrhosis or HCC can be made non-invasively after exclusion of all other possible causes and in the presence or history of metabolic risk factors.
- Patients with features suggestive of severe liver disease/NASH or significant fibrosis or cirrhosis/HCC require further evaluation and management.
Step 8: Liver biopsy in NAFLD
Liver biopsy is indicated in NAFLD patients suspected of having NASH on non-invasive assessment and in the presence of a co-existing liver disease.
Algorithmic approach for the evaluation of patients with NAFLD
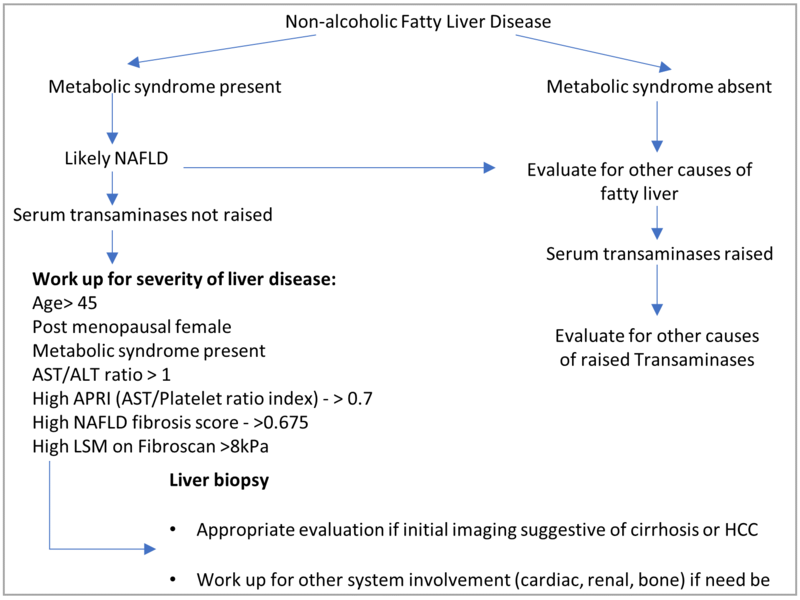
AST: aspartate aminotransferase; ALT: alanine aminotransferase; APRI: AST/platelet ratio index; LSM: liver stiffness measurement
Treatment of Non-cirrhotic Non-alcoholic Fatty Liver Disease (NAFLD)
Since NAFLD is a lifestyle disease, therapeutic modalities in patients with NAFLD include lifestyle modifications such as weight loss and exercise and control of risk factors such as diabetes mellitus, hyperlipidaemia and hypertension. Pharmacological treatment is indicated only in select situations.
Most of the liver society guidelines would recommend the use of either vitamin E or pioglitazone in biopsy proven patients with NASH with or without diabetes mellitus. In addition, many new pharmacological agents are being evaluated in various phase III studies across the globe. Because of the low risk of liver-related complications in patients without NASH, indiscriminant use of pharmacological treatment is not recommended in these patients.
Management of patients with NAFLD
Step 1: Control of metabolic risk factors
- Control of overweight or obesity with diet + exercise:
- All patients with NAFLD irrespective of their body weight should be advised regular exercise and those who are overweight and obese are advised weight reduction. Regular exercise has been shown to improve insulin sensitivity even without weight reduction and in fact is the only treatment for patients with NAFLD without overweight/obesity/central obesity (lean NAFLD).
- The exercise regimen should consist of brisk walking, jogging, cycling or rhythmic aerobic exercises for a minimum of 45 min/day, at least 5 days per week, to achieve a target heart rate of 70 to 80% of the maximal heart rate (calculated by subtracting age in years from 220).
- Weight reduction in overweight/obese patients should be slow and sustained with initial target of weight reduction being 10% of the body weight over a period of 6 to 8 months.
- Various dietary regimens are available but severe hypo-caloric diets are not recommended in NAFLD. If available, it is suggested to involve a dietitian for the dietary advice. Overall, patients who are overweight or obese need to create a negative balance by consuming fewer calories (30% reduction in calorie intake recommended by restricting both carbohydrates and fats) and burning more calories by regular exercise.
- Patients with NAFLD should avoid any amount of alcohol intake.
- Bariatric surgery is not recommended as a primary treatment of NAFLD/NASH. If otherwise indicated (because of severe obesity and associated metabolic conditions), bariatric surgery has been found to improve liver histology in patients with NAFLD/ NASH. Data on the use of intra-gastric balloon as an intermediate treatment of obesity (in between lifestyle modifications and bariatric surgery) is still evolving.
- Control of Diabetes mellitus/hypertension/dyslipidaemia: Because of the systemic nature of the illness, patients with NAFLD are best managed by a multi-disciplinary approach. There are no contraindications for the use of medications to control diabetes mellitus, hypertension or dyslipideamia. In particular, statins if indicated are also safe in patients with NAFLD having raised transaminases.
Step 2: Metabolic risk factors- absent
Exercise (as detailed earlier)
Step 3: Pharmacological treatment for NASH
- Only two drugs (Vitamin E and Pioglitazone) are recommended by most of the scientific societies for use in non-diabetic patients with biopsy proven NASH. Side effect profile and the long term safety of both vitamin E and Pioglitazone are still in question.
- New drugs in the pipeline include Farnesoid X receptor agonist obeticholic acid, dual peroxisome proliferator activated receptor (PPAR) agonists [alpha and delta (Elafibranor) and alpha and gamma (Saroglitazar)], Liraglutide, a long acting glucagon like peptide -1 agonist, Cenicriviroc, a chemokine, probiotics and fecal microbiota transplantation (FMT).
Management of NASH related cirrhosis and HCC
Management of patients with NASH related cirrhosis and HCC including the indications for transplantation are not different from patients of other etiologies of cirrhosis and HCC.
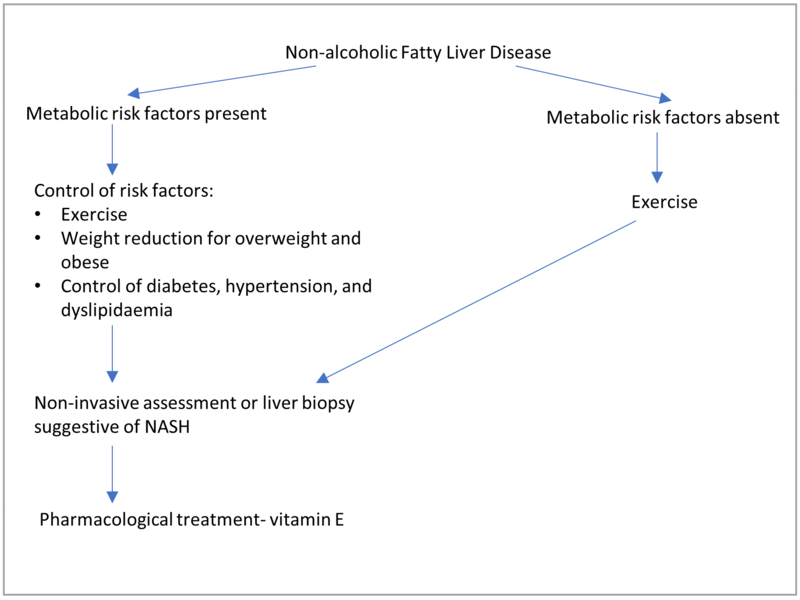
Algorithmic approach for the treatment of patients with NAFLD
This article was originally published on October 14, 2019.
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
The author, Dr. Ajay Duseja is a Professor with the Department of Hepatology, PGIMER, Chandigarh.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries