Residual ASCVD risk: What are the potential drivers? - Dr Arun Kochar
M3 India Newsdesk Mar 07, 2022
This article highlights the identification of residual risk factors that may help in better initiation of treatment and help in the management of patients with atherosclerotic cardiovascular disease (ASCVD).
Residual risk in ASCVD patients
There has been enhanced morbidity and mortality in patients of atherosclerotic cardiovascular disease despite adequate compliance with the current evidence-based guideline-directed care. It has been seen that there is a risk of cardiovascular events and or progression of existing disease in spite of the optimal control of the risk factors. So, the risk of future cardiovascular events is not completely eliminated even though there had been the best efforts of physicians and patients. Residual risk term is usually applied to secondary prevention cohort.
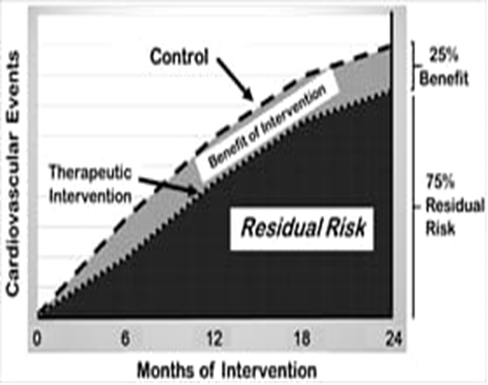
Cardiovascular events despite best available lipid-lowering therapy resulting in 25% reduction in events at 2 years
These residual risk factors are often unrecognised and not addressed in routine clinical practice settings. Various statin and PCSK9 (Proprotein convertase subtilisin/Kexin type 9) inhibitor trials have conclusively shown that despite aggressive LDL lowering risk there was of events still remains. [1]
For example, despite the ultra-low reduction achieved with the FOURIER (Further Cardiovascular Outcomes Research with PCSK9 Inhibition in Subjects with Elevated Risk) and ODYSSEY OUTCOMES (Evaluation of Cardiovascular Outcomes After an Acute Coronary Syndrome During Treatment With Alirocumab) trial showed residual risk may be due to other atherogenic lipid subfractions that are not modified with PCSK9 inhibition, high baseline risk and or involvement of other metabolic and prothrombotic factors.
For example, it was identified that in the FOURIER trial, the recurrent cardiovascular event rate at 3 years in patients treated with PCSK9i remained high at 9.8%.[2] Thus despite the treatment of LDL-C is considered as the cornerstone of risk reduction, however, there are other potential drivers of ASCVD which can be categorised into three pathways.[3]
Pathways of residual cardiovascular risk
| Residual risk | ||
| Residual inflammation risk | Residual metabolic risk | Residual thrombotic risk |
| Colchicine- COLCOT, Canakinumab- CANTOS, Statins- JUPITER | Icosapent ethyl-REDUCE IT, SGLT2 inhibitors DAPA-HF, EMPA-REG, GLP1 RA LEADER, SUSTAIN-6 | Riveroxaban-COMPASS, Dual antiplatelets- PEGASUS TIMI-54 |
Residual inflammatory risk
Pro-inflammatory biological pathways may play a key role in atherogenesis. There exists a strong link between lipid and inflammation. The accumulation and oxidation of LDL-C at intimae tend to promote inflammation and drive atherosclerosis.[4]
Results from the clinical trials of JUPITER, PROVE-IT TIMI 22, and ASCOT LLA demonstrate that serum levels of hsCRP are important in defining the residual cardiovascular risk in high-risk individuals with hypercholesterolemia.[5] The concept of residual inflammatory risk was also validated in the CANTOS trial.[6] Apart from hsCRP, other molecules like IL-1 and IL-6 also play a key role in atherosclerosis.
Residual thrombotic risk
In patients with established ASCVD, anti-platelet agents become essential for optimal medical management. Though Aspirin was used, the risk of serious vascular events remained in the clinical trial settings.[7] Adding low-dose anti-coagulation to antiplatelet therapy have yielded benefits in the ATLAS ACS-2, TIMI-51 and COMPASS clinical trials.
In the ATLAS AC2 TIMI-51, it was identified that in patients with acute coronary syndrome, the addition of rivaroxaban to antiplatelet therapy demonstrated a 16% relative risk reduction in major adverse cardiovascular events.[8] Similarly, in the COMPASS clinical trial, low-dose rivaroxaban plus aspirin vs. aspirin alone resulted in a 24% reduction in the primary outcome and a 22% reduction in the net clinical endpoint.[9]
Residual metabolic risk
1. Lipoproteins- As increased levels of lipoprotein are associated with increased risk of MI, Lp(a) could be a strong predictor of residual risk in patients who are on statins. Evolocumab was associated with a 26.9% reduction in the Lp(a) levels. The role of Lp(a) in reducing the residual cardiovascular risk is still an area of investigation.[3]
2. Triglycerides- There also exists debate whether triglycerides should be targeted to improve CV outcomes. In the JELIS trial, supplementation with EPA and statins had shown a significant reduction in the major coronary events. [10]
3. Diabetes- GLP-1 and SGL-2 inhibitors have shown improvement in CV outcomes. In the DAPA-HF study, SGL2-i demonstrated benefits in individuals without diabetes, particularly in patients with heart failure and reduced ejection fraction.[11]
Click here to see references
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
The author, Dr. Arun Kochar is a Senior Interventional Cardiologist practising in Mohali.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries