Proteinuria: Evaluation & Management for Improved Kidney Health
M3 India Newsdesk Jun 27, 2023
Proteinuria is an excessive protein in the urine. In this article, the author covers the causes, evaluation, and treatment options for elevated urine protein levels. Discover the pathophysiology, diagnostic approach, and targeted therapies for improved kidney health.
Proteinuria
Proteinuria is a routine finding in day-to-day practice in both outpatients as well as inpatients. Proteinuria can be physiological as well as pathological which requires further investigation, especially in the setting of co-morbidities like diabetes mellitus.
Proteinuria, in conjunction with estimated glomerular filtration rate (eGFR), is now utilised in the classification of chronic kidney disease (CKD). The degree of proteinuria correlates with disease progression.
Definitions
- Proteinuria is a comprehensive expression employed to indicate the presence of various proteins, such as albumin, globulin, Bence-Jones protein, and mucoprotein, in the urine. It serves as a general term encompassing the existence of urinary proteins.
- The typical amount of protein excreted in urine is less than 150 mg within a 24-hour period, primarily comprising secreted proteins like Tamm-Horsfall proteins.
- The average rate of albumin excretion in a normal individual is 5-10 mg per day, while an albumin excretion rate exceeding 30 mg per day is considered abnormal.
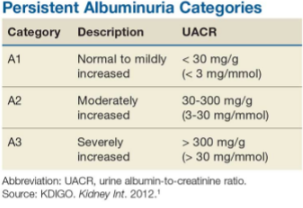
- In the past, moderately and severely increased albuminuria was referred to as microalbuminuria and macroalbuminuria, respectively.
- If albuminuria persists for 3 months, it is classified as chronic kidney disease (CKD). Nephrotic-range proteinuria is defined as the excretion of more than 3.5 g of protein in the urine within a 24-hour period.
Aetiology and classification
Proteinuria can be classified as transient and persistent.
Transient proteinuria (Benign causes/physiological)
- Urinary tract infection
- Orthostatic proteinuria (occurs after the patient has been upright for a prolonged period, absent in early morning urine)
- Fever
- Heavy exercise
- Vaginal mucus
- Pregnancy
Persistent proteinuria (Pathological causes)
- Primary renal disease
- Glomerular (such as glomerulonephritis)
- Tubular
- Secondary renal disease
- Diabetes mellitus
- Connective tissue diseases
- Vasculitis
- Amyloidosis
- Myeloma
- Congestive cardiac failure
- Hypertension
Pathophysiology
Proteinuria is a result of three different pathways, including:
- Glomerular dysfunction
- Tubulointerstitial disease
- Secretory proteinuria
- Overflow proteinuria
1. Glomerular dysfunction
This is the most common cause of proteinuria. The altered permeability of the glomerular basement membrane due to glomerular dysfunction leads to the presence of albuminuria and immunoglobinuria. This dysfunction results in urinary protein excretion exceeding 2 g per 24 hours.
Causes of glomerular dysfunction include:
- Diabetic nephropathy (most common)
- Drug-induced nephropathy (NSAIDs, lithium, heavy metals, heroin)
- Lymphoma
- Infections (HIV, hepatitis B, and C)
- Primary glomerulonephropathies
- Amyloidosis
- Malignancies
- Connective tissue diseases such as SLE
2. Tubulointerstitial dysfunction
This is due to the dysfunction at the proximal tubule, resulting in the impairment of the uptake of filtered proteins. Tubulointerstitial dysfunction typically results in milder proteinuria compared to glomerular dysfunction, with 24-hour urine protein levels below 2 grams.
Most of the protein reabsorption occurs in the proximal convoluted tubules. This reabsorption in the proximal convoluted tubules has a transport maximum which, when reached, can result in proteinuria.
Causes of tubular dysfunction include:
- Hypertensive nephrosclerosis
- NSAIDs induced nephropathy
- Nephrotoxins
- Chronic tubulointerstitial disease
3. Secretory proteinuria
Secretory proteinuria results from the over-secretion of specific proteins in the tubules, the most notable one being the Tamm-Horsfall proteins in interstitial nephritis.
4. Overflow proteinuria
Excessive production of proteins can overwhelm the reabsorption capacity of the proximal convoluted tubules, resulting in proteinuria. Overflow proteinuria occurs when the plasma concentration of low-molecular-weight proteins goes beyond the tubular capacity to reabsorb the filtered proteins.
Causes of overflow proteinuria include:
- Multiple myeloma
- Myoglobinuria
- Amyloidosis
Diagnostic approach
History taking and physical evaluation
History of pedal oedema, facial puffiness, frothing in urine, hematuria, burning micturition, rashes, oral ulcers, joint pain, and especially drug history should be taken.
Physical examination from head to toe is a must, especially for oedema, respiratory crackles and rashes.
To begin with, urinary tract infections and diabetes mellitus should be excluded. Urine dipsticks are the first screening tests for proteinuria that can be performed easily. This is a semi-quantitative test in addition to being a qualitative test.
In order to quantify the degree of proteinuria, a 24-hour urine collection is cumbersome. An easier and more reliable alternative is the spot urine protein to creatinine ratio (UPCR) from a single specimen, which should preferably be the early morning urine sample.
Along with assessing protein levels, it is important to evaluate serum electrolytes, urea, and creatinine. For a nephrotic range of proteinuria with more than 3.5 g/24-hours or a UPCR of more than 350 mg/mmol, the serum albumin levels and cholesterol concentrations should be checked.
Other tests
- Autoantibody determinations - including ASO titers, ANA, anti-dsDNA antibodies, complement levels (C3 and C4), anti-phospholipase A1 receptor autoantibody, and cryoglobulins
- Hepatitis B and C and HIV serologies
- Urine and plasma protein electrophoresis for light chains
- Anti–glomerular basement membrane (anti-GBM) antibodies and antineutrophil cytoplasmic antibodies (ANCA)
Imaging studies
- Renal ultrasonography to review the size and echogenicity of the kidneys and for any obstructive uropathy.
- Chest radiography or computed tomography may also be indicated in cases of suspected vasculitis.
Renal biopsy
It should be especially considered in acute renal worsening settings with the nephritic or nephritic syndrome to diagnose any potentially reversible cause earlier.
Indications for renal biopsy
- Nephrotic Syndrome: In older children and adults differentiate between Minimal Change Disease, Focal Segmental Glomerulosclerosis (FSGS) and Membranous Nephropathy.
- Nephritic Syndrome: Presence of dysmorphic RBC in urine, cellular cast.
Treatment
The treatment of proteinuria is mainly focused on treating the specific underlying cause. Most treatment modalities focus on reducing the degree of proteinuria. These include drugs acting on the renin-angiotensin-aldosterone system.
The Kidney Disease Improving Global Outcomes (KDIGO) guideline strongly recommends using ACE inhibitors or angiotensin receptor antagonists (ARB) in adults with more than 300 mg/24 hours of persistent proteinuria.
In diabetic nephropathy, SGLT2 inhibitors are now considered the cornerstone for not only reducing proteinuria but also retarding CKD progression In cases of active vasculitis or any other auto-immune conditions; steroids or other immune-suppressive treatment may be required.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Bhavin Mandowara is a practising nephrologist at Zydus Hospital, Ahmedabad.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries