Prevention and Management of Dengue Fever During Monsoon Season
M3 India Newsdesk Aug 15, 2024
This article outlines the key aspects of dengue, including its transmission methods, prevention strategies, and detailed guidelines for managing the disease at different stages.
Dengue is a mosquito-borne viral disease and is a major public health concern throughout tropical and subtropical regions of the world. In India, cases peak from July to November, following the monsoon season.
Transmission
Dengue viruses are primarily transmitted through the bite of infected female Aedes mosquitoes, specifically Aedes aegypti and Ae.albopictus.
While transmission typically occurs through mosquito bites, there have been reports of dengue transmission through blood transfusion and organ transplantation, as well as congenital dengue infections in neonates born to mothers infected late in pregnancy.
Prevention of dengue
Ae. Aegypti likes to sleep in cool, shaded areas and have strong anthropophilia. It breeds on stagnant water, laying eggs on the inner walls of the water containers above the waterline. The eggs stick to the walls and take about 7-10 days to develop into an adult mosquito.
Dengue can be prevented by reducing the breeding of vector mosquitoes or by preventing mosquito bites.
A. Reducing the breeding of vectors
- Ae. aegypti breeds almost entirely in domestic man-made water receptacles found in and around households (water storage containers, water reservoirs, overhead tanks, desert coolers, industrial and domestic junk, construction sites, etc.) Whereas Ae. albopictus prefers natural larval habitats (tree holes, latex collecting cups in rubber plantations, leaf axils, bamboo stumps).
- Aedes mosquitoes don’t fly very long distances and thus spend their lives in smaller blocks. So reducing stagnant water in and around the house can greatly reduce the number of mosquitoes in the neighborhood.
B. Preventing bites
Aedes aegypti is predominantly a day feeder and therefore precautions should be advised at all times of the day.
- Wearing protective clothing
- Using mosquito repellents
- Using mosquito nets while sleeping
Clinical features of dengue
Dengue fever presents as an acute febrile illness lasting 2-7 days, with symptoms such as:
- Headache
- Retro-orbital pain
- Myalgia
- Arthralgia
- Rash
Later during the critical illness, the patient may develop-
- Haemorrhagic manifestations
- Thrombocytopenia or leucopenia
- Warning signs and symptoms
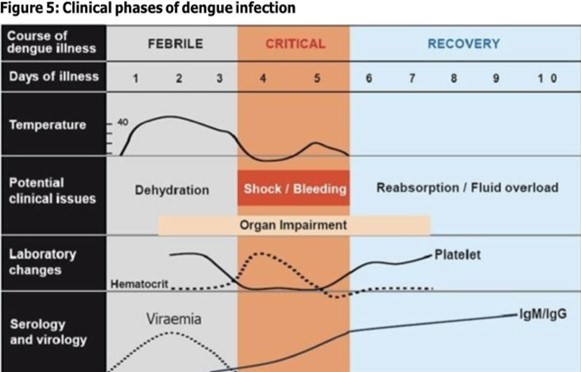
A. Febrile phase
This phase usually lasts for 2-7 days
- Fever: High grade, maybe biphasic.
- Headache.
- Myalgias and arthralgia.
- Rashes: the initial rash is typically a flushing erythema within 24-48 hours of onset of symptoms which evolves into a morbilliform rash characteristically described as “ white islands in a sea of red” sparing the palms and soles.
- Bleeding manifestations: may be observed in this phase. The majority of cases may manifest as vaginal or gastrointestinal bleeding, as well as skin and mucosal haemorrhage; hematemesis, melena, and excessive menstrual bleeding are less typical presentations.
- Epistaxis, or hematuria.
- Physical examination: may reveal facial puffiness, conjunctival congestion, pharyngeal erythema, lymphadenopathy, and hepatomegaly( small). It is also essential to look for petechiae (on the skin and palate) and bruising(particularly at venipuncture sites) and perform a tourniquet test.
B. Critical phase (leakage phase)
5-10% of patients progress to the critical phase which usually lasts for 24-48 hours.
Commonly seen in patients who have a history of previous dengue infection or in patients with comorbidities.
Vasculopathy and coagulopathy, which cause plasma leakage and bleeding and ultimately result in shock and organ dysfunction, are the hallmarks of this phase. Clinicians need to be careful in recognising and observing the warning signs of the critical phase at the early stage.
Warning symptoms and signs
- Persistent vomiting
- Abdominal pain and tenderness
- Lethargy and/or restlessness, sudden behavioural changes
- Bleeding manifestations like epistaxis, melena, haematemesis, excessive menstrual bleeding, and haematuria
- Syncope or giddiness
- Clinical fluid accumulation (ascites and pleural effusion)
- Enlarged Liver(>2cm)
- Laboratory: A sharp decline in platelet count accompanied by a progressive increase in haemoglobin.
C. Convalescent phase (Recovery phase)- Lasts for 2-3 days
With the timing and optimal management during the critical phase patients start recovering and pass through the recovery phase. The majority of the patients from the febrile phase also pass through this recovery phase for the complete cure.
In this recovery phase, the extracellular fluid lost to capillary leakage returns to the circulatory system during the recovery phase, and signs and symptoms improve. This phase occurs after the critical phase.
The patient gets a convalescent rash that spares normal skin in places and is characterised by confluent erythematous eruption.It is often pruritic. If fluid replacement is not carefully optimised, the patient may develop pulmonary oedema as a result of fluid excess.
Severity of dengue
A. Dengue without warning signs (Mild dengue/Group A)
involves patients with fever and other non-specific symptoms but no warning signs.
B. Dengue with warning signs and/or Risk factors (Moderate dengue/ Group B)
Here the patient presents with a fever with warning symptoms and signs. This usually occurs near the end of the febrile phase and preferably at defervescence.
C- Severe dengue (Group C)
These individuals are those who have developed symptoms and indicators of shock, plasma leakage, and organ dysfunction after developing mild to moderate dengue.
Manifestations of severe dengue
- Severe plasma leakage leading to:
- Shock
- Fluid accumulation with respiratory distress
- Severe bleeding (as evaluated by the treating team).
- Severe organ dysfunction ( renal failure, metabolic acidosis).
- ≥1000 units/L of either alanine aminotransferase (ALT) or aspartate aminotransferase (AST).
- Impaired consciousness (GCS < 9).
Management of dengue
A. Management of Mild dengue patients (Group A)
Both the patients and their family members should be instructed regarding the following at the outpatient department.
- Educate about warning signs and report if they appear.
- Red spots and patches on the skin
- Bleeding from nose and gums
- Severe abdominal pain and persistent vomiting
- Black tarry stools
- Drowsiness or irritability
- Pale, cold or clammy skin
- Difficulty in Breathing
- Advice to stay away from fizzy drinks and drink enough ORS or coconut juice orally.
- The patient needs to take adequate bed rest.
- Body temperature should be kept below 100°F. If the temperature goes beyond 100°F, give paracetamol.
B. Management of moderate dengue patients (GroupB)
- Should be admitted for in-hospital management.
- Baseline haematocrit (HCT) test should be performed before starting fluid therapy.
- Every cautionary indication and symptom needs to be closely watched.
- Encourage oral fluids. If not tolerated, start intravenous fluid therapy of 0.9% NS or RL.
- Adequate intravenous fluid volume may be required to maintain good perfusion and urine output of about 0.5 ml/kg/hour.
- Give 7-10ml / kg crystalloid solution (Hartmannʹs or 0.9% NSS) in 1 h.
- Evaluation of clinical improvement should be done every hour.
- Fluid reduction should be done gradually as follows if the patient's circumstances improve (blood pressure, pulse pressure, Hct lowered, urine output improved, capillary refilling time improved):
- 5–7 mL/kg/h for 2–4 hours
- 3–5 mL/kg/h for 2–4 hours
- 2-4 mL/kg/h for 2–4 hours
Depending on the patient's clinical condition, fluid should be discontinued after 24 to 48 hours.
C. Management of severe dengue patients
Judicious IV fluid resuscitation is essential and lifesaving.
Choose a crystalloid solution (0.9% NS or RL) that will keep the blood flowing during the plasma leakage period, which lasts for around 24 to 48 hours.
Blood transfusion should be given to patients with established severe bleeding, or suspected severe bleeding (fall in Hct) with unexplained hypotension.
Transfuse platelet only if bleeding is present or Prophylacticaly platelet transfusion may be considered for counts < 10,000/cumm without bleed.
Fluid therapy
The action plan for treating patients with compensated shock is as shown in the algorithm below:
- Start intravenous fluid resuscitation with isotonic crystalloid solutions at 10- 20ml/kg/hour over one hour.
- If the patient’s condition improves, intravenous fluids should be gradually reduced to 7–10 ml/kg/hr for 1–2 hours, then to 5–7 ml/kg/hr. for 1-2 hours, then to 3–5 ml/kg/hr. for 2-4 hours, followed by 2-3 ml/kg/h for 2-3 hours, and after that, based on the state of your heart, for an additional 2-3 hours, and for as long as 24–48 hours.
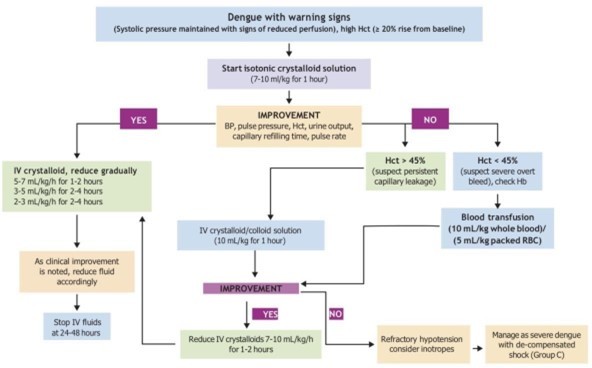
Patients who are in hypotensive or decompensated shock need to be treated more aggressively.
The action plan for treating patients with hypotensive shock is as shown in the algorithm below:
- Start intravenous fluid resuscitation with a bolus of 20 ml/kg of crystalloid or colloid solution (if available) spread out over 15 minutes.
- Give a 10 ml/kg/hr crystalloid/colloid infusion for one hour if the patient's condition improves. Next, keep up the crystalloid infusion and progressively cut back.
- If shock persists, review the haematocrit. If the haematocrit increases or is still high (>45%), repeat a second bolus of crystalloid solution at 10-20 ml/kg over 15-30 minutes.
- If there is improvement following this second bolus, lower the rate to 7–10 ml/kg/hr for one to two hours, and then carry out the previously described gradual reduction of fluid. Up to three rapid boluses may be given.
- If hematocrit decreases compared to the initial reference hematocrit (<40% in children and adult females, <45% in adult males), this indicates bleeding and the need to cross-match and transfuse blood as soon as possible. Transfusion of whole blood (10 ml/kg) or packed red blood cells (5 ml/kg) should be given.
If the shock is refractory:
- The use of inotropes should be considered.
- Determine cardiogenic shock and septic shock.
- Evaluate metabolic causes and organ dysfunction.
- Evaluate concomitant medical conditions and stabilise the baseline condition.
- Evaluate persistent acidosis and risk of (hidden) haemorrhage and treat accordingly.
Conclusion
Understanding and managing dengue involves a comprehensive approach to prevention, early recognition of symptoms, and appropriate clinical management based on the severity of the disease. By reducing mosquito breeding sites and preventing mosquito bites, along with timely medical intervention, the impact of dengue can be significantly mitigated.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr. Apurva Jain is an MBBS, DNB Family Medicine, DAA working as a Senior resident in ESI hospital, Delhi.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries