Practice points for Hypoglycaemia treatment in type 2 diabetes: Dr. Raveendran AV
M3 India Newsdesk Oct 21, 2019
Fear of hypoglycaemia is a major factor which prevents not only the healthcare providers but also people with diabetes from timely up-titration of medication to achieve strict glycaemic control. Here Dr. Raveendran AV offers key practice points for treatment.
Key messages
- Patient awareness regarding symptoms of hypoglycaemia and self-treatment options reduces the risk of progression to severe hypoglycaemia
- In people with mild hypoglycaemia, follow “15-15 rule” that is to give 15 grams of carbohydrate orally and check blood sugar after 15 minutes. If still found low repeat the treatment
- In patients with severe hypoglycaemia, parenteral glucose or glucagon should be started without delay
Type 2 diabetes is a common lifestyle disorder with a worldwide prevalence of 424.9 million in 2017and is expected to increase to 628.6 million by the year 2045 as per the IDF guideline.Various professional bodies advice tight glycaemic control in addition to control of other cardiovascular risk factors to reduce diabetes related complications.
We have an armamentarium of drugs to control blood glucose level, yet, majority of our patients are not achieving treatment targets. Fear of hypoglycaemia is a major factor which prevents not only the healthcare providers but also people with diabetes from timely up-titration of medication to achieve strict glycaemic control.
Hypoglycaemia
Symptoms of hypoglycaemia can be classified as neuroglycopenic and autonomic. Hypoglycemia if not recognised and treated in time can result in brain damage, seizure, coma and death.
- Symptoms due to sympathetic adrenal activation:
- Sweating
- Anxiety
- Tremor
- Nausea
- Palpitation
- Tachycardia
- Symptoms due to Neuroglycopenia:
- Fatigue
- Dizziness
- Headache
- Visual disturbances
- Drowsiness
- Difficulty speaking
- Inability to concentrate
- Abnormal behaviour
- Confusion
- Loss of consciousness
- Seizures
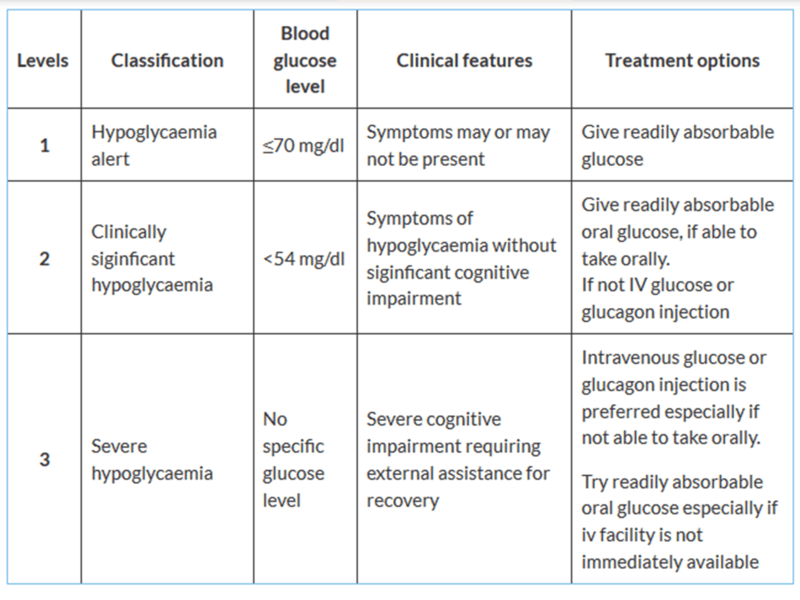
In simple words any hypoglycemia which is self treated is called mild or moderate hypoglycaemia and those episodes which require external assistance is called severe hypoglycaemia. If only autonomic symptoms are present it is called mild hypoglycaemia and if both autonomic and neuroglycopenic symptoms are present and still patient does not require external assistance it is called moderate hypoglycaemia. Depending upon the blood sugar value and the presence of cognitive impairment, hypoglycaemia is divided into 3 levels.
Levels and treatment options
How frequent is it?
- In type 1 diabetes mild hypoglycaemia is reported twice in a week on an average, whereas severe hypoglycaemia occurs 1 to 1.7 episodes per patient per year.
- In type 2 diabetes the overall incidence of severe hypoglycaemia is 0.02 episodes per patient per year.
When people with type 2 diabetes become insulin deficient the risk of hypoglycaemia approaches that of type 1 diabetes. In comparison with type 1 diabetes, people with insulin treated type 2 diabetes developing severe hypoglycaemia are more likely to require assistance of emergency medical team.
The reported incidence of hypoglycaemia misses a major fraction because most of the time it is not reported, especially mild or moderate hypoglycaemia and asymptomatic hypoglycaemia will be detected only with continuous blood glucose monitoring.
Pathophysiology and precipitating factors
When there is an imbalance between anti-diabetic medication intake, food intake, or physical exertion, blood glucose level drops down resulting in hypoglycaemia. Secretion of counter regulatory hormones like glucagon, epinephrine, cortisol and growth hormone helps to correct hypoglycaemia.
Risk of hypoglycaemia depends on the hypoglycaemic risk of anti-diabetic medication and individuals ability to secrete counter regulatory hormone. Mismatch of anti-diabetic medication or insulin timing, amount, reduced oral intake, alcohol intake, vomiting or drug dispensing errors are the most common immediate precipitating cause of hypoglycaemia.
Risk of hypoglycaemia associated with anti-diabetic medication
- High risk
- Sulfonlyurea; HbA1c reduction (%): 1 - 2
- Insulin
- Moderate risk
- Glinide; HbA1c reduction (%): 0.5 -1
- Mild or no risk
- Metformin; HbA1c reduction (%): 1 -2
- Thiazolidinediones; HbA1c reduction (%): 0.5 - 1.4
- Alpha-glucosidase inhibitors; HbA1c reduction (%): 0.5 - 0.8
- GLP-1RA; HbA1c reduction (%): 0.5 - 1
- SGLT-2i; HbA1c reduction (%): 0.5 - 1
- DPP-4i; HbA1c reduction (%): 0.5 - 0.8
- Pramlintide; HbA1c reduction (%): 0.25 - 0.5
Risk factors
- In people with type 2 diabetes mellitus treated with insulin, the risk of hypoglycaemia increases with duration of diabetes, duration of insulin therapy (especially for those with more than 10 years), HbA1c concentration and glucose variability.
- Risk factors for severe hypoglycaemia in people with sulfonylurea treated type 2 diabetes include age, past history of vascular disease, renal disease, reduced intake of foods, alcohol consumption and interaction with other drugs.
- Risk of hypoglycemia is increased by the presence of autonomic neuropathy, gastroparesis (where peak insulin action occurs before food is absorbed because of gastroparesis) and renal disease (reduce insulin clearance loss of renal contribution to gluconeogenesis).
- In patients with diabetes impaired cognitive function is associated with the risk of severe hypoglycaemia. Prior episode of severe hypoglycaemia itself is a risk factor for further hypoglycaemic episodes.
- Prolonged hypoglycaemia is seen in those taking long-acting sulfonylurea, in elderly or with defective counter regulatory hormone release.
Symptoms of hypoglycaemia become less intensive in older age group. In the younger age group, symptoms of hypoglycaemia occurs well before the occurrence of cognitive dysfunction and the difference in the threshold is about 1.0mmol/L (18 g/L) whereas in older individuals symptoms and cognitive dysfunction occurs together, limiting the time available for corrective action, resulting in severe hypoglycaemia and related complications.
Glycaemic threshold for the secretion of glucagon and epinephrine is found to be low in older individuals compared to younger. The magnitude of glucagon and epinephrine response to hypoglycaemia is lower in elderly at mild hypoglycaemia but equal in both younger and older age group at moderate and severe hypoglycaemia.Insulin clearance is also low in elderly age group resulting in increased risk of hypoglycaemia.
- In people with type 2 diabetes, counter regulatory hormone release occurs at higher blood glucose level compared to non-diabetic states and in people with type 1 diabetes
- In people with type 2 diabetes having insulin deficiency, there is acquired defect in the counter regulatory response to hypoglycaemia
Drugs and hypoglycaemia
Beta blockers prolong hypoglycaemia by inhibiting compensatory mechanisms. It also masks the warning signs of hypoglycaemia like palpitation and tremor. Lithium, high dose aspirin and theophylline potentiate the effect of insulin, sulfonylureas resulting in hypoglycaemia. ACE inhibitors, chloroquine, disopyramide, quinolones etc. can also induce hypoglycaemia.
Clinical significance
Impaired consciousness and convulsions associated with severe hypoglycaemia can result in fall, bony injury and general friability especially in the elderly. In addition to this, hypoglycaemia can precipitate major vascular events like stroke and myocardial infarction which is associated with high morbidity and mortality. Acute heart failure and ventricular arrhythmia associated with hypoglycaemia can be life threatening.
Severe hypoglycaemic episodes in people with type 2 diabetes are associated with increased risk of dementia. Severe hypoglycaemia affects the quality of life by direct effect of hypoglycaemia and also by the fear of recurrence of hypoglycaemia. Those who develop hypoglycaemic episodes are sometimes reluctant to escalate anti-diabetic medication dose, even when blood glucose level is poorly controlled.
Hypoglycaemia unawareness
In people with recurrent hypoglycaemia, there is defect in the sympatho-adrenal response to hypoglycaemia, resulting in impaired counter regulatory hormone response and impaired awareness of hypoglycaemia, which is called hypoglycaemia associated autonomic failure (HAAF). Hypoglycaemic unawareness (HU) is less common in people with type 2 diabetes compared with type 1 diabetes.
Impairment in symptom awareness of hypoglycaemia increases the risk of subsequent severe hypoglycaemia by 6-fold and 9-fold in people with type 1 and type 2 diabetes respectively.
There is a vicious cycle of hypoglycaemia and hypoglycaemic unawareness. Avoidance of hypoglycaemia for few weeks improves counter regulatory hormone response and hypoglycaemic unawareness.
Treatment of hypoglycaemia
Hypoglycaemia is a medical emergency. Early recognition and treatment is very important. The general principle of hypoglycemia management is to give rapidly absorbable oral glucose in patients who can take oral, and parenteral glucose in those not able to take orally.
Start treatment at hypoglycaemia alert value of 70 mg/dl or less. Give 15 grams of glucose orally in mild or moderate hypoglycaemic episodes. Examples of common sources of readily absorbable glucose are:
- 125 ml or 4 oz apple juice or orange juice (do not give orange juice to renalpatients)
- 125 ml or 4 oz regular sugar-sweetened cola
- 185 ml or 6 oz sugar-sweetened ginger ale
- 3 BD glucose(contain 5 g of carb per tablet) tablets
- 4 Dex4 glucose (contain 4 g of carb per tablet) tablets
- 15 mL (3 teaspoons) or 3 packets of table sugar dissolved in water
- 15 mL (1 tablespoon) of honey
Check blood glucose level after 15 minutes after consumption of 15 gram of carbohydrates and if found to be low repeat the treatment again. This is called “15-15 rule” that is to give 15 grams of carbohydrate and check blood sugar after 15 minutes.
Pure glucose is preferred, but any carbohydrate containing food intake improves blood glucose level. The acute glycemic response correlates well with glucose content. Fat present in the food may delay the glycemic response. Protein present in the food increases insulin response and hence carbohydrate with high protein content should not be used to treat hypoglycaemia. Patients with hypoglycaemia should be advised to eat a meal or snack after correction of hypoglycaemia to prevent recurrence. Hypoglycaemia in people taking alpha glucosidase inhibitor must use glucose as it inhibits the digestion and absorption of polysaccharides and oligosaccharides.
In patients with severe hypoglycaemia give 30 to 50 ml of 50% dextrose bolus followed by infusion of 5D or 10 D to maintain blood glucose level more than 100 mg/dl.
Parenteral glucagon 1 mg can be administered intravenously (I.V) or intra-muscularly (I.M). Vomiting is an uncommon side effect of glucagon therapy and patient has to be kept in lateral position especially if unconscious.
Glucagon therapy mobilises glycogen from liver and increase blood glucose by about 36 mg/dl within 15 minutes.
Parenteral glucagon emergency kits (1 mg) should be made available and patient and care takers has to be taught how to administer it. Usually it is given subcutaneously (S/C) or intramuscularly (IM) over the buttock, arm or thigh.
Glucagon therapy is less effective in:
- Undernourished patients
- Patients with severe liver disease
- Repeated hypoglycaemia
- Oral hypoglycaemic agent induced hypoglycaemia
Counter regulatory hormonal response and exogenous glucose administration can result in high blood glucose level for hours in patients following severe hypoglycaemic episode.
After correction of hypoglycaemia, in all cases, the healthcare provider should look for:
- Precipitating cause of hypoglycaemia
- Missed meal
- Dosage error
- Increased exercise
- Alcohol use
- Deliberate overdose
- Hypoglycaemic 'warning symptoms' in the patient
Precipitating cause of hypoglycaemia has to be addressed and necessary changes have to be made in the anti-diabetic medication prescription and glycemic targets. Look for warning symptoms of hypoglycaemia and identify those who are having hypoglycaemic unawareness.
Prevention of hypoglycaemia
- Take food and anti-diabetic medications in time
- Avoid unplanned extreme physical exertion
- Carry glucose tablets, juice or food containing readily absorbable sugar
- Wear identification card stating the diabetic status and risk of hypoglycaemia
- Avoid alcohol. Alcohol induces hypoglycaemia by
- Hepatic glycogen depletion
- Inhibition of gluconeogenesis
- Decreased food intake after consumption of alcohol
- Alcohol induced gastritis and vomiting
In patients with recurrent hypoglycsemia or other associated risk factors, glycaemic targets should be individualised in order to reduce complication.
All patients should receive health education regarding hypoglycaemia and medication dose adjustments have to be done if needed.
Conclusion
Hypoglycemia is common in people with diabetes. In addition to early recognition and treatment of hypoglycemia, identification of precipitating causes, modification of the anti-diabetic medication dosage schedule, identification of hypoglycemic unawareness and individualization of treatment targets are important in people with diabetes developing hypoglycemia.
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
The author, Dr. Raveendran AV is a past Asst. Professor from Govt. Medical College, Kozhikode, and is currently a Specialist in Internal Medicine in the Sultanate of Oman.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries