Posterior Urethral Valves [PUV] Obstruction in Children
M3 India Newsdesk Jul 25, 2024
This article discusses Posterior Urethral Valves (PUV), a cause of bladder outlet obstruction in male children, highlighting the need for early detection and long-term management to prevent severe renal complications.
Posterior Urethral Valves
Posterior Urethral Valves [PUV] is a form of bladder outlet obstruction in male children. Other causes of bladder outlet obstruction in children include the anterior urethral valve, urethral stricture and diverticulum and obstructing masses including bladder polyps and prolapsing ureteroceles.
In bladder outlet obstruction both ureters and kidneys are dilated as a result of secondary VUR which can result in end-stage renal failure and therefore the need for urgent decompression. Posterior urethral valves are congenital and should be suspected in antenatally detected bilateral hydronephrosis.
An appropriate delivery plan must be instituted in such children to reduce further renal damage. Most neonates with PUV have already sustained significant damage to kidneys and urinary tract and therefore require long-term management.
Incidence
The incidence of PUV is around 1 in 5000 to 1 in 8000 male live births. The presentation is usually of a distended bladder with bilateral hydronephrosis. However, the hydronephrosis can be unilateral on occasions providing a blow-out effect. Also, the hydronephrosis or the kidney can rupture producing urinomas or ascites. In a study on 25 patients with PUV, the mortality rate was 12% and 17% of the patients required renal transplantation at the mean age of 6.5 years [1].
Aetiology
- The exact aetiology of PUV is not clear. During embryogenesis posterior urethral folds develop around 4 weeks of gestation and fail to obliterate resulting in bladder outlet obstruction.
- However, a different theory suggesting the persistence of a membrane between the verumontanum and the anterior part of the posterior urethra produces varying levels of obstruction. Young described three types of PUV in 1919 [2], and various modifications have been developed since then.
Diagnosis
- The majority of the cases of PUV are suspected antenatally on ultrasound imaging. Bilateral hydronephrosis associated with a thickened urinary bladder and a reduced amniotic fluid can all suggest PUV.
- In severe cases, as reduction of amniotic fluid is required for adequate lung development pulmonary hypoplasia develops.
- After delivery, clinically the child does not pass urine and laboratory blood tests may reveal high serum creatinine levels suggesting renal failure. Postnatal renal and bladder ultrasound can pick up findings as mentioned earlier with antenatal scans.
- MCUG is diagnostic and reveals a dilated posterior urethra proximal to a narrowing in the urethra [Figure].
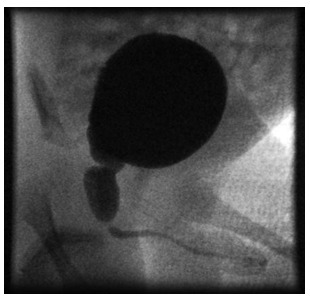
Figure: MCUG in a neonate showing dilatation of posterior urethra with proximal narrowing suggesting posterior urethral valves.
Direct visualisation of the PUV is possible with cystoscopy and therapeutic fulguration or ablation valves can be achieved simultaneously.
Management
Immediate decompression of the bladder along with adequate resuscitation is the immediate management. Protecting the upper tracts and kidney function is most important.
Associated renal injury should be assessed with regular ultrasound scans and nuclear imaging with DMSA to determine the renal function. Long-term prophylactic antibiotics should be started to reduce the risk of further UTI and further renal damage.
In an attempt to empty the urine through a blocked urethra the bladder hypertrophies and dysfunctions. Subsequent to bladder decompression bladder dysfunction might persist and is seen in more than 50% of the patients [3].
The sensory innervations of the bladder and posterior urethra are altered and therefore these patients cannot empty the bladder regularly. Urodynamic studies are necessary to evaluate bladder dysfunction.
Although most patients respond to conservative measures, there is a wide spectrum of patients ranging from complete resolution of bladder dysfunction to failure of bladder function. The worry is that these patients can later develop a worse condition called valve bladder syndrome.
The syndrome includes:
- A thick-walled and noncompliant urinary bladder
- Urinary incontinence
- Persistent dilation of the upper urinary tracts
- Polyuria (secondary to renal dysfunction)
In patients with valve bladder syndrome, regular CIC is essential to keep the bladder empty thereby minimising the injury to upper tracts along with reducing the risk of further UTIs.
In a study on 18 boys with valve bladder syndrome, along with regular daytime Clean intermittent catheterisation [CIC], nocturnal bladder emptying was recommended and was shown to result in prompt and impressive improvement or elimination of hydronephrosis in these and similar groups of patients (Koff et al, 2002) [4].
Suprapubic catheters can be inserted to reduce the trauma of regular CIC and in patients with poor compliance. Further surgery like bladder augmentation and mitrofanoff could be considered if bladder function fails to improve. Circumcising the foreskin can benefit these patients. In a study on 78 patients with PUV, the incidence of UTI reduced by 83% following circumcision [5].
The GFR at one year of age is the most important predictor of future CRF development. The onset of proteinuria during the follow-up is associated with a worse prognosis [6].
Related article:
Pelvic-Uteric Junction [PUJ] Obstruction in Children
Vesico Ureteric Junction [VUJ] Obstruction in Children
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Sivasankar Jayakumar is MBBS, MRCS, FEBPS, Department of Paediatric Surgery & Urology, Apollo Cradle & Children’s Hospital, Karapakkam, Chennai.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries