Polycystic Ovary Syndrome: Management Strategies
M3 India Newsdesk Nov 11, 2024
This article explores the role of nutrition in managing PCOS, focusing on evidence-based nutritional interventions that can aid hormonal balance and fertility, particularly for women in clinical settings.
Polycystic Ovary Syndrome (PCOS) is one of the most common endocrine disorders in women of reproductive age, affecting both hormonal balance and fertility. Hyperandrogenism, menstrual irregularities, and polycystic ovaries characterise the condition. It can lead to insulin resistance, obesity, and other metabolic disturbances, further complicating the patient's health.
One of the most effective strategies for managing PCOS is dietary modification, which can positively impact hormonal regulation and improve fertility outcomes.
The role of insulin resistance in PCOS and fertility
Insulin resistance is a hallmark of PCOS, affecting approximately 70% of women with the condition. It not only contributes to weight gain but also exacerbates hormonal imbalances, including elevated androgens (testosterone), which disrupt ovulation and fertility.
Dietary approach:
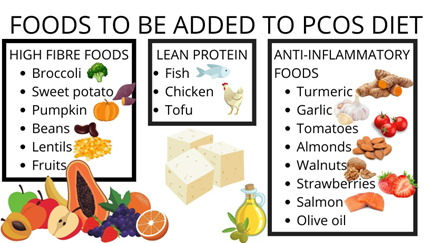
A low glycemic index (GI) diet, which focuses on whole grains, legumes, and non-starchy vegetables, can help manage insulin resistance. Patients should aim to:
- Carbohydrate intake: Limit simple carbohydrates to <45% of total daily calories.
- Fiber intake: Increase to 25-30 grams per day to improve insulin sensitivity.
- Protein: Ensure that 20-25% of the daily calorie intake comes from lean proteins like fish, chicken, and plant-based options such as lentils.
Reducing androgen levels through diet
Elevated androgen levels are a key cause of hirsutism and acne in PCOS patients, as well as anovulation, which impacts fertility. Insulin resistance drives these elevated levels, so addressing this through diet can help.
Dietary approach
A diet rich in anti-inflammatory foods can support hormone regulation. Patients should focus on:
- Omega-3 fatty acids: 1-2 servings per week of fatty fish such as salmon, mackerel, or supplements.
- Antioxidants: Include colourful vegetables and fruits (e.g., berries, spinach, and bell peppers) to reduce inflammation.
- Processed foods and trans fats: Avoid processed meats, sugary drinks, and foods high in trans fats, which can increase androgen production.
Weight management: A key to hormonal balance
Even a modest weight loss of 5-10% can restore ovulation in many women with PCOS, improving fertility outcomes. Obesity exacerbates insulin resistance, which worsens hormonal imbalances.
Dietary approach
- Calorie deficit: Patients should aim for a daily calorie reduction of 500-750 kcal, leading to a gradual weight loss of 0.5-1 kg per week.
- Balanced macros: A well-balanced diet consisting of 40% carbohydrates, 30% protein, and 30% healthy fats.
- Physical activity: Encourage 150 minutes of moderate physical activity per week to improve weight loss and insulin sensitivity.
The role of micronutrients in PCOS
Certain micronutrients are essential for hormonal balance and fertility in women with PCOS. Deficiencies in Vitamin D, magnesium, and folate are commonly seen in women with the condition.

Dietary approach
- Vitamin D: Encourage supplementation of 1000-2000 IU/day, especially in regions where sunlight exposure is limited. Foods like fortified dairy, eggs, and mushrooms can also help.
- Magnesium: 300-400 mg/day of magnesium through foods like leafy greens, nuts, and seeds.
- Folate: Essential for women trying to conceive, ensure a daily intake of 400-800 mcg of folate through sources like lentils, beans, and fortified cereals.
Addressing fertility challenges through diet
Fertility struggles are common in women with PCOS due to irregular ovulation or lack of ovulation. Restoring hormonal balance through diet can help regulate menstrual cycles and improve ovulation rates.
Dietary approach
- Low-carb diets: Studies show that a diet containing <45% of total daily energy from carbohydrates can enhance ovulation.
- Inositol supplementation: Clinical research supports the use of inositol (2-4 grams daily) to improve ovulation and reproductive outcomes in women with PCOS.
- Fertility-enhancing foods: Zinc-rich foods (pumpkin seeds, chickpeas) and antioxidants (berries, nuts) support reproductive health.
Case study 1: Restoring ovulation through dietary change
A 32-year-old woman diagnosed with PCOS, presented with irregular periods and difficulty conceiving. Her BMI was 30, and she exhibited insulin resistance.
Intervention
The patient was placed on a low glycemic index diet, with a focus on increasing her intake of fiber, lean proteins, and healthy fats. She was advised to reduce her intake of processed foods and sugary drinks while increasing physical activity.
Outcome
Within six months, the patient experienced a 15% reduction in body weight, and her menstrual cycles became more regular. After nine months, she was able to conceive naturally without the need for fertility treatments.
Case study 2: Managing insulin resistance and androgen levels
A 28-year-old woman with PCOS, experiencing hirsutism and acne. Blood tests revealed elevated androgen levels and insulin resistance.
Intervention
The patient was prescribed a diet rich in anti-inflammatory foods, including omega-3 fatty acids, and was advised to avoid high-sugar and processed foods. She also started supplementing with inositol and Vitamin D.
Outcome
After four months, the patient saw a significant improvement in her skin, reduced facial hair growth, and better insulin sensitivity. Her androgen levels returned to normal, and her ovulation patterns improved.
Conclusion
- Managing PCOS through dietary interventions is not only effective in controlling symptoms but also plays a significant role in restoring hormonal balance and improving fertility.
- By addressing insulin resistance, androgen levels, and inflammation through a balanced, nutrient-dense diet, women with PCOS can see significant improvements in both metabolic and reproductive health.
- As healthcare providers, it is crucial to guide patients on the benefits of dietary modification in PCOS management.
- Personalised nutrition plans, combined with lifestyle changes, can lead to better long-term outcomes and improved quality of life for these patients.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
The author of this article: Ms Rutambhara Nhawkar is a Clinical Dietician, M. Sc. (Clinical Nutrition & Dietetics), Certified Diabetes Educator and a medical writer from Pune.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries