Overview of Allergic Rhinitis and its Management
M3 India Newsdesk Sep 14, 2023
This article discusses the classification, symptoms, diagnosis, and treatment of allergic rhinitis, an inflammatory illness of the nasal mucosa brought on by environmental allergens. It also highlights the disorder's rising prevalence and detrimental effects on quality of life.
Definition & burden of allergic rhinitis
- Allergic rhinitis is an inflammatory process of the nasal mucosa, typically IgE-mediated, elicited by environmental allergens and characterised by the presence of inflammatory cells within the mucosa and submucosa. The course of the disease involves one or more of the symptoms enumerated below, persisting for at least one hour a day for at least two consecutive days, which are reversible spontaneously or with treatment. The symptoms include nasal discharge, nasal itching, sneezing and nasal obstruction.
- Rising prevalence is seen not only in children but also in adults.
- Makes up to 55% of all allergy cases in India.
- Is the most common allergy encountered in clinical practice in India.
- Around 30 percent Indian population suffers from allergic rhinitis.
Allergic rhinitis has a profound negative impact on the quality of life of patients and their families.
It is also a major cause of school and work absenteeism.
it is vital to ensure timely and correct diagnosis and implement appropriate management based on the latest international or national guidelines.
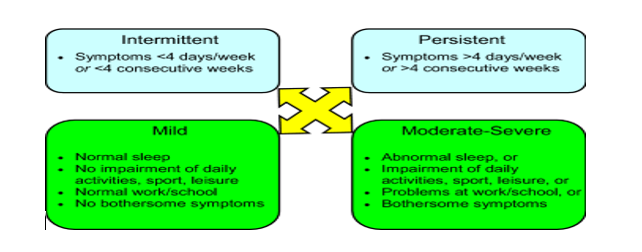
Classification of allergic rhinitis
- According to duration and severity
- According to allergen-causing symptom
Seasonal allergic rhinitis (SAR) - It develops only during specific periods of the year (corresponding to the pollination of wind-pollinated plants or mould sporulation).
Perennial allergic rhinitis (PAR) - It occurs when the condition is triggered by allergens found in the patient’s environment at concentrations sufficient to induce symptoms of the disease all year round.
Episodic allergic rhinitis (EAR) - It is caused by exposure to a specific airborne allergen on a sporadic and short-term basis.
- According to pathophysiology
- IgE mediated – most common (90%)
- Non- IgE medicated
Symptoms of allergic rhinitis
- Sneezing
- Nasal itching
- Rhinorrhea
- Nasal congestion
- Post nasal drainage
- Smell disturbances
- Headache and facial pain
- Ear and ear symptoms
Untreated allergic rhinitis can lead to
- Asthma
- Sinusitis
- Otitis media
- Upper respiratory tract infection
- Nasal polyp
Diagnosis of allergic rhinitis
1. History is the most important.
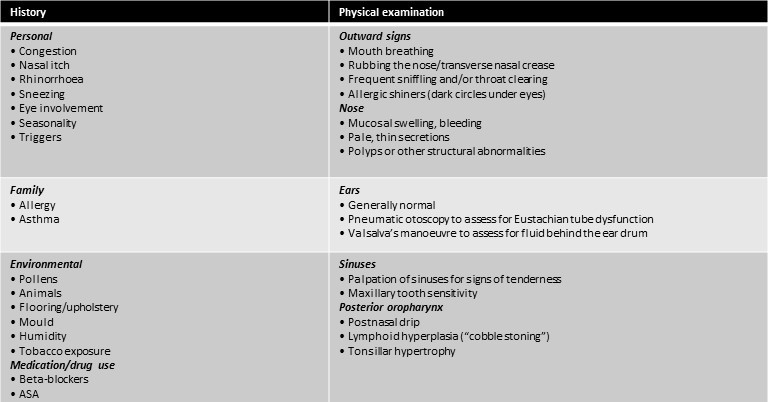
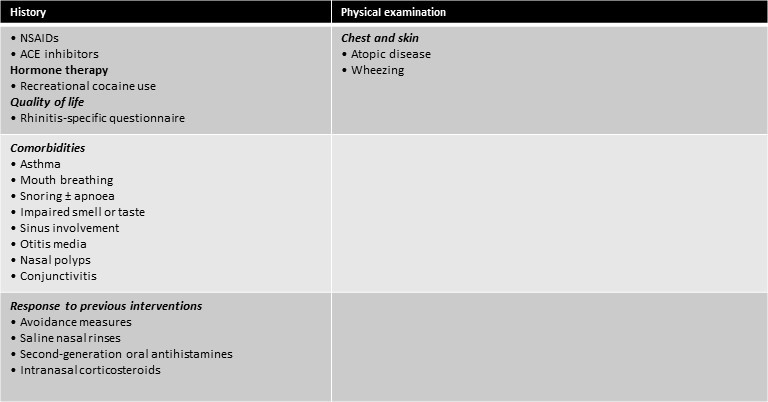
2. Skin prick allergy testing is beneficial to identify allergens in seasonal allergic rhinitis and to decide further treatment and avoidance.
3. Basic blood report- CBC WITH ESR, S. TOTAL IgE.
4. Nasal endoscopy or CT to rule out complications.
5. Pulmonary function test- to rule out asthma.
Management of patient
1. Education of patients (in children and also their caregivers) is the most important.
2. Avoidance of allergens and irritants (possible in SAR)
The first-line treatment of allergic rhinitis involves the avoidance of relevant allergens (e.g., house dust mites, moulds, pets, pollens) and irritants (e.g., tobacco smoke).
Pollen and outdoor mould exposure can be reduced by keeping windows closed, using window screen filters, using an air conditioner, and limiting the amount of time spent outdoors during peak pollen seasons. For patients allergic to animal dander, removal of the animal from the home is recommended.
3. Pharmacotherapy
The most important drug categories include:
- Glucocorticoids (GC): Intranasal, oral
- H1 receptor antagonists (second-generation H1-antihistamines – AH) (oral – AHpo, intranasal – AHin)
- Antileukotrienes (ALTR) (in children mainly montelukast)
- Ipratropium bromide (intranasal)
- α-sympathomimetics (intranasal, oral)
- Saline solutions (intranasal)
- Anti-IgE antibodies (subcutaneous)
- Cromones (intranasal)
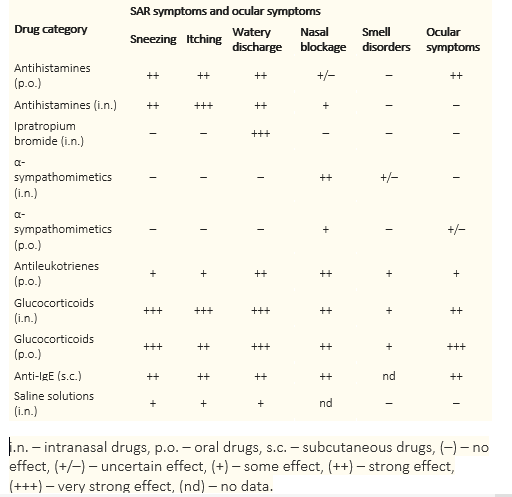
- The most common initial choice of drug is an intranasal steroid (fluticasone furoate or mometasone) with a combination of oral antihistaminic plus antileukotrines (Levocetirizine/ bilastine/ fexofenadine with montelukast).
- Duration of treatment is decided by the severity of symptoms of allergen immunotherapy (sublingual or subcutaneous, effective particularly in SAR).
4. Allergen immunotherapy (sublingual or subcutaneous, effective particularly in SAR)
- Allergen immunotherapy involves the subcutaneous administration of gradually increasing quantities of the patient’s relevant allergens until a dose is reached that is effective in inducing immunologic tolerance to them.
- Allergen immunotherapy is an effective treatment for allergic rhinitis, particularly for patients with intermittent (seasonal) allergic rhinitis caused by pollens, including tree, grass and ragweed pollens. It has also been shown to be effective for the treatment of allergic rhinitis caused by house dust mites, Alternaria, cockroaches, and cat and dog dander.
- Allergen immunotherapy should be reserved for patients in whom optimal avoidance measures and pharmacotherapy are insufficient to control symptoms or are not well tolerated. Since this form of therapy carries the risk of anaphylactic reactions, it should only be prescribed by physicians who are adequately trained in the treatment of allergy and who are equipped to manage possible life-threatening anaphylaxis.
Conclusion
- Allergic rhinitis is a common disorder that can significantly impact patient quality of life.
- The diagnosis is made through a comprehensive history and physical examination. Further diagnostic testing using skin-prick tests or allergen-specific IgE tests is usually required to confirm that underlying allergies cause the rhinitis.
- The therapeutic options available for the treatment of allergic rhinitis are effective in managing symptoms and are generally safe and well-tolerated. Second-generation oral antihistamines and intranasal corticosteroids are the mainstay of treatment for the disorder.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr. Nisarg Patel (UGC), MD Pulmonology, Omkar Chest Care and Medical Hospital, Ahmedabad.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries