Oncology and Artificial Intelligence
M3 Global Newsdesk Nov 05, 2023
Oncology is benefiting greatly from AI, especially in the areas of cancer diagnosis, screening, and data management. However, healthcare professionals are concerned about issues related to bias, data quality, and the possible loss of human touch in patient care.
Artificial intelligence (AI) is making rapid advancements in medicine, including oncology with ChatGPT, perhaps, grabbing the most headlines of the day. But for all its promise and potential, AI has also unleashed a wave of less savoury sentiments in the medical community, from apprehension and scepticism to outright mistrust, and even fear.
A global survey was conducted with 50 practising oncologists about their interests, knowledge, and experience with AI in their work settings. Of the respondents, 63.4% worked in medical oncology, 19.5% in radiation oncology, and 17.1% in haematology-oncology, with the vast majority working in urban and suburban settings.
The results provide a snapshot of clinicians’ views on AI's benefits and limitations today, how they see AI's role in cancer care in the future, and whether they believe it will ultimately improve patient outcomes.
The current state of AI in oncology
Back in 2012, when IBM launched its landmark Watson for Oncology program, the notion of AI digital assistants—dare we call them robots?—seemed like the stuff of science fiction.
Although Watson was largely unsuccessful, AI-driven tools are now notably impacting various areas of oncology—from enhancing early detection and diagnosis through sophisticated imaging and screening algorithms to rapidly analysing and managing vast amounts of healthcare data for better HCP efficiency.
One thing we know from our survey data: Today's oncologists are clearly intrigued by this burgeoning technology—nearly all of our survey respondents (95%) indicated they were somewhat or very interested in AI’s potential use in the diagnosis and treatment of cancer.
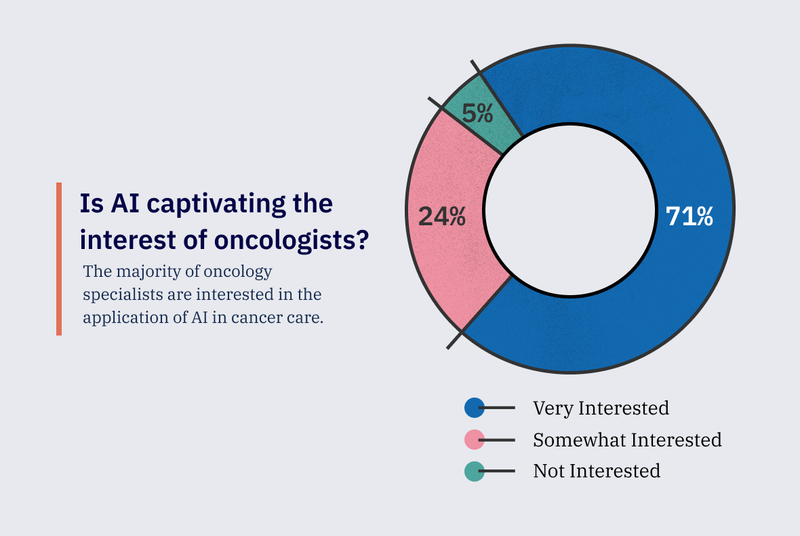
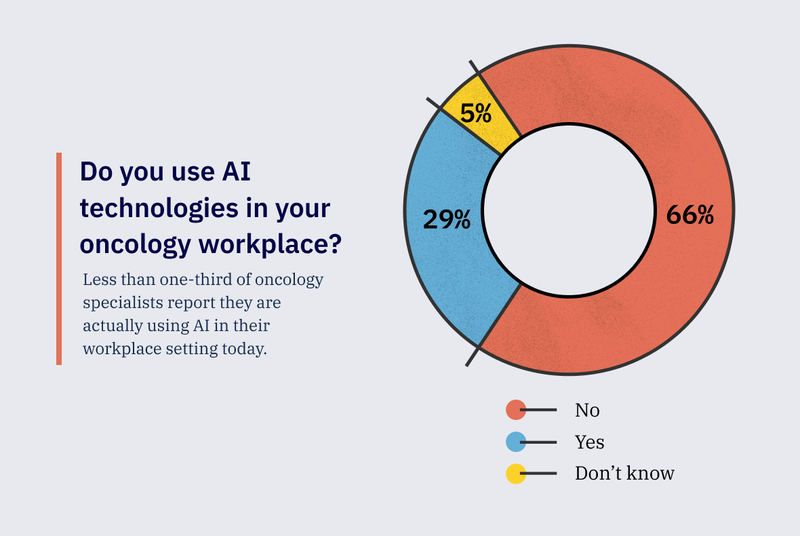
On the other hand, while new AI devices and software are already proving successful in the field, less than one-third of oncology specialists surveyed are currently using AI technologies in their practice.
Definitions
Algorithm: A blueprint for computers to process information and make decisions based on given criteria.
Machine learning (ML): A subset of AI that enables computers to learn and improve their performance by analysing data and identifying patterns without explicit programming or human intervention.
Deep learning: An advanced form of ML that uses multi-layered artificial neural networks inspired by the human brain to process data and make decisions. This technology excels at handling complex data sets and can automatically identify intricate patterns, making it well-suited for tasks like image and speech recognition.
Natural language processing (NLP): A field within AI that focuses on the interaction between computers and human language, enabling machines to understand, interpret, and generate human language.
Where is AI's impact most visible in oncology?
Cancer diagnosis—radiology and pathology specifically—are the areas where AI is having the most impact, according to experts.
"The most developed component of AI in oncology is diagnosis optimisation. We're now using computer vision to help us find more things in pathology slides," says Arturo Loaiza-Bonilla, MD, MSEd, FACP. Dr. Loaiza-Bonilla is the medical director of oncology research at Capital Health in Pennington, New Jersey, and is on the faculty at Drexel University College of Medicine.
"In radiology, on average, a radiologist must interpret an image every three to four seconds to maintain the daily workflow. Clinicians also experience sustained inattentional blindness," he said.
"AI is driving efficiency and accuracy in this field by helping check images faster and detecting objects our eyes can't perceive."
— Arturo Loaiza-Bonilla, MD, MSEd, FACP
Dr Loaiza-Bonilla's observation about the areas seeing the most impact from AI aligns with research. A 2022 analysis of AI-based, FDA-approved devices found cancer radiology to be the field with the largest number of AI devices—accounting for 54.9% of approved devices, followed by pathology with 19.7%.
This popularity is mirrored in practice. Studies have revealed that some hospitals and point-of-care centres are already using radiologic AI products successfully. Moreover, radiologists who utilise AI in their practices are generally satisfied with their experience and gain value from its use. In fact, the majority of radiologists and residents anticipate substantial changes in the radiology profession over the next decade.
Cancer screening, detection, and diagnosis
According to the American Cancer Society, screening mammograms fail to identify around 1 in 8 breast cancers and about half of the women who get screenings over a 10-year period will have a false-positive finding.
In an August 2023 study published in The Lancet, researchers conducted a clinical safety analysis of an AI-supported screen-reading protocol, compared with standard screen reading by radiologists following mammography.
"AI-supported mammography screening resulted in a similar cancer detection rate compared with standard double reading, with a substantially lower screen-reading workload, indicating that the use of AI in mammography screening is safe."
— Authors, The Lancet
In an earlier study, Google's AI system's performance was tested on mammograms of more than 25,000 women in the UK and 3,000 in the US. The 2020 study results indicated that Google's AI could identify breast cancers about as accurately as radiologists while reducing false positives by 5.7% in the US group and 1.2% in the UK group. When compared with the original radiologists' diagnoses, Google’s AI reduced the number of missed cases by 9.4% in the US group and 2.7% in the UK group.
In 2021, the FDA approved Paige Prostate, an AI pathology tool designed to screen prostate biopsies and identify areas with a high likelihood of cancer. According to the FDA's news release at the time, prostate cancer detection improved by 7.3% on average when pathologists were assisted by the AI tool compared with when pathologists were unassisted.
AI's areas of promise and potential
Data management and analysis
Data organisation is the component of oncology where AI has the most promise now, according to Dr Loaiza-Bonilla.
NLP tools provide a rich opportunity to uncover valuable insights into care quality and patient outcomes. Around 80% of medical data stays unstructured and untapped after its creation. NLP tools can parse and transform unstructured text (clinical notes) from EHR data into actionable information, a process that would otherwise require significant and time-consuming manual effort.
"These tools give us more efficiency in our daily workflow—helping us spend less time looking for sources of patient information or organising patient data siloed in disparate platforms."
— Arturo Loaiza-Bonilla, MD, MSEd, FACP
Finally, researchers should use all available data to further advance precision oncology and enhance understanding of our complex biological systems, according to Dr. Loaiza-Bonilla. Datasets—omics, sequencing, EHRs—are continually increasing in volume, dimensionality, and complexity. AI has proven itself to be the only feasible means of continuing to collect, manage, and accurately analyse the ever-growing volume of health data.
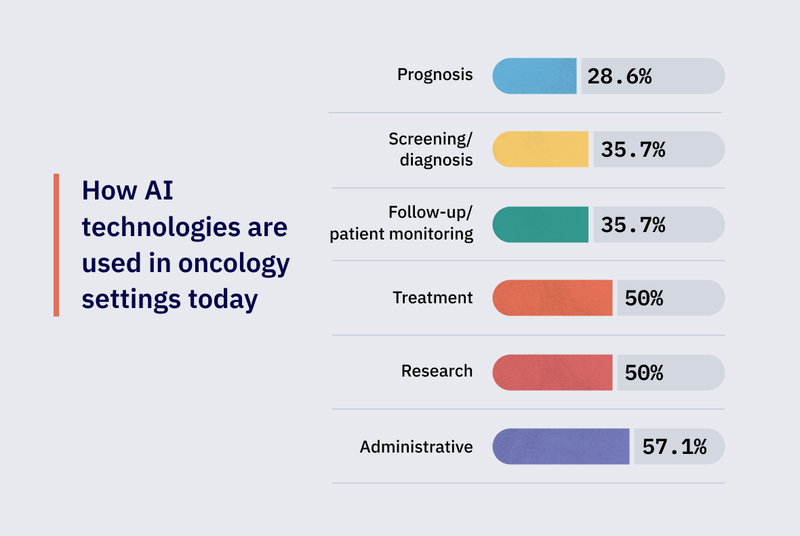
According to the global survey, AI is primarily being used in current oncology practices for administrative tasks, treatment, and research. (Forty-four per cent of our respondents work in an academic setting; 37% in independent clinics; and the remaining 20% in a hospital-owned outpatient cancer centre.) Surveyed physicians note diagnostic confidence, diagnostic speed, and the streamlining of monotonous tasks and administrative burdens as the most significant enhancements.
Related: ChatGPT: The clinician’s new tech assistant?
Treatment planning, outcomes prediction, and monitoring
Researchers have been looking into using AI in image-based cancer treatment planning by developing algorithms that automatically segment tumours and healthy tissues in medical images.
These algorithms are then used to create 2D or volumetric models of the tumour and surrounding tissues, which can be used to plan radiation treatment.
An FDA-approved software that does this is the VBrain, which detects brain metastases and conducts segmentation for stereotactic radiosurgery.
Imaging-based ML models may also enable the prediction of future cancer outcomes, such as locoregional recurrence, distant recurrence, and mortality. For instance, different emerging image-based ML models can predict clinical outcomes such as overall survival and disease-free survival for pancreatic cancer patients.
In the future, this information may power post-treatment surveillance and recurrence prevention strategies. Finally, using similar techniques as in cancer detection and diagnosis, AI can potentially monitor tumours—determining their stability or progression.
Precision medicine
Precision medicine applications for cancer typically rely on the detection of specific genetic variations and alterations. Now, AI tools are being developed to identify specific gene mutations from tumour pathology images as an alternative to traditional genomic sequencing that typically requires invasive biopsies. They are also accelerating drug discovery.
Related: Is AI-driven drug discovery the next big thing?
Challenges and limitations of AI in oncology
Data access and quality
Despite these benefits, concerns remain. AI relies on vast amounts of data, and the first hurdle in developing AI-based oncology tools is data accessibility. There's a lack of structured, cancer-related health data and standardisation in the collection, storage, and sharing of existing structured health data in and between EHRs and digital health tools.
Getting quality data to develop and train AI-based models also poses a challenge. Data from retrospectively acquired datasets are usually the easiest to amass. Still, questions around their purity for use are raised because predetermined inclusion and exclusion criteria might lead to unconscious biases in newly developed AI algorithms.
Practitioner concerns
"As clinicians, we're rightfully worried about the AI ‘black box’ phenomenon, which is basically that we don't know what's behind the algorithm," Dr. Loaiza-Bonilla says about HCP concerns that may hinder adoption. "How can we be sure that the decision process taking place is fully vetted by a professional with the requisite healthcare/patient care expertise?"
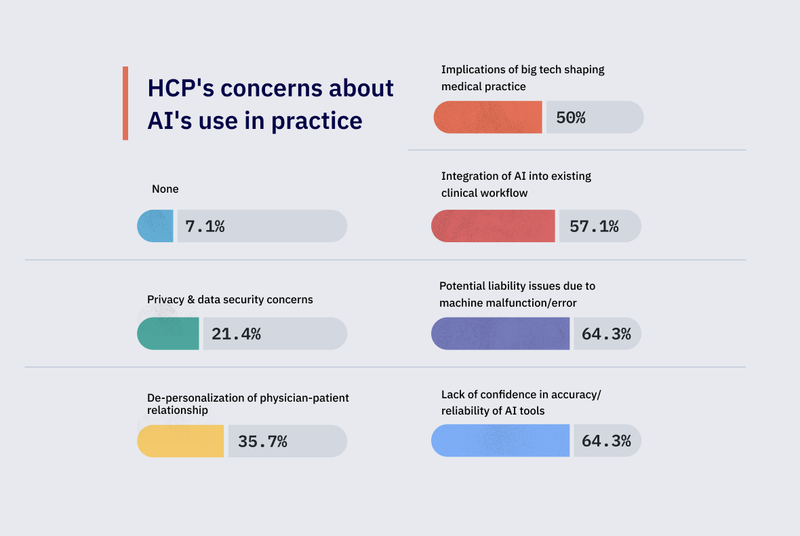
The global survey data mirrors these concerns, with 64.3% of respondents citing accuracy and reliability as a concern of integrating AI into clinical practice, and 64.3% citing liability issues. Finally, half of the respondents are concerned about the implications of major tech companies shaping current and future healthcare practices.
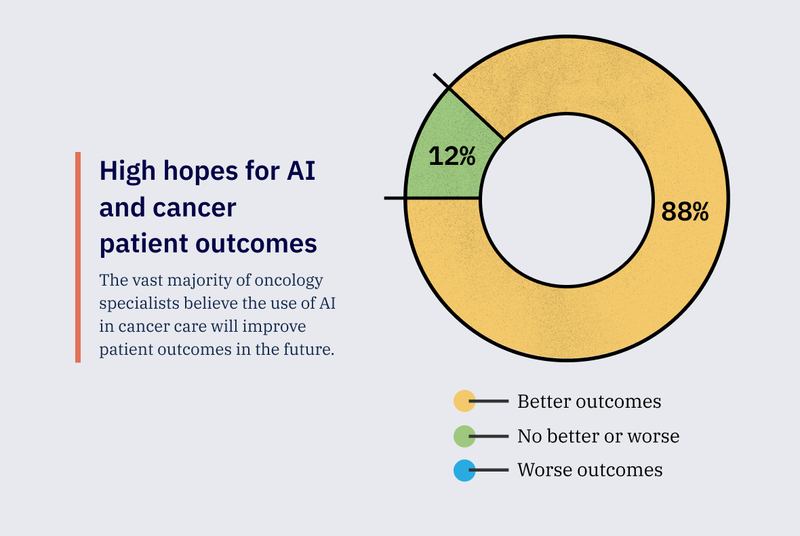
Even so, the majority of global survey respondents (87.7%) believe AI in oncology will lead to better patient outcomes.
Clinicians may not be the only ones concerned with the potential for an algorithm to skew the facts—their patients could harbour these fears as well. Or worse, they may not even know AI is being used in their care. Approximately 60% of the physicians surveyed believe their patients are aware of AI tools being used in their oncological care; 36% were not sure.
What we heard from HCPs: Ethical concerns
- You are removing the human factor—AI currently makes up answers if it doesn't find what you want to know in the real world.
- Replacement of human-to-human interaction; replacement of healthcare workers.
- Patient data privacy and security.
- Human interaction/empathy still has a role to play.
- We should always double-check AI’s work, to make sure no mistakes or errors were made.
- AI utilising my voice when calling patients.
- Potential for insurance fraud, and data mining for profit from the AI company.
- An AI decision is based on the data you provide but may lack the full picture for that decision.
- Validity of AI-based treatment recommendations.
- Maintaining evidenced-based practice.
- People supervising AI who shouldn't be.
- Bias and fairness, informed consent, transparency and accountability, and patient autonomy.
Regulatory challenges
Integrating AI tools and devices in medical care delivery presents many regulatory challenges. Key challenges include:
- Establishing appropriate validation processes
- Determining evidentiary standards
- Addressing the dynamic nature of AI to evolve with continuous data input
- Maintaining transparency in decision-making
Additionally, regulatory agencies must tackle data privacy and security issues, and minimise the risks of bias and discrimination that could stem from inadequate or unrepresentative training data.
Currently in the US, the FDA classifies software intended to treat, diagnose, cure, mitigate, or prevent disease or other conditions as a medical device. Most AI-enabled products that fall under this medical device classification are specifically categorised as either Software as a Medical Device (SaMD) or Software in a Medical Device. However, a gap exists because there is AI-enabled software utilised in healthcare and life sciences excluded from the definition of a medical device and consequently not subject to the FDA's authority.
Ethics and bias
Several challenges must be addressed to minimise bias and facilitate fairness in AI-powered oncology tools.
“The potential for bias in using AI in oncology really comes into play with clinical decision support tools. Does the AI tool take into account demographics that could affect outcomes?" Dr. Loaiza-Bonilla questions.
"It's always going to be important to include the right population of patients when building AI models. For instance, are we taking datasets from only fully insured patients or persons working or living around academic centres and using them as the ground benchmark? That may not reflect the population of patients living in more rural areas without access to clinical trials or even genomic testing, who may also be underinsured."
Integrating AI into oncology practice
AI use in oncology is still in its infancy. The majority of studies and research centres around developing valid methods and not integrating these methods into clinical practice. There's still a long way to go in validating these methods, finding effective pathways for the clinical integration of the tools, educating clinicians on their benefits and disadvantages, and thoroughly assessing associated outcomes and costs.
What HCPs need for successful AI integration
- An effective understanding of the limitations and pitfalls of AI.
- Training for how to phrase questions so AI doesn't give made-up answers.
- Data management skills, collaboration skills to effectively communicate with AI, ethical considerations, and continuous learning.
- Hands-on clinical training to help incorporate AI into practice.
- Privacy training.
- Training regarding the use and integration into practice, especially with treatment algorithms and imaging scan interpretation.
- Not to ignore the human touch of AI.
- PhD in computer science if you really want to know how AI works, and what problems to anticipate.
- Demonstrated the value of AI in improving diagnosis and treatment.
- Proper data input awareness of misinformation possibilities in AI output.
- Training regarding the processes, logistics, and methodology—data extraction and synthesis is key to utilising AI in medical practice.
- How to be vigilant about potential errors.
Future outlook
Three-quarters of the physicians surveyed reported they expect AI technologies to become an “essential” part of their everyday practice, and the vast majority cited optimism for AI's role in cancer care in the future.
But others report concerns over the lack of human input.
"AI currently makes up answers if it doesn't find what you want to know in the real world."
— Global survey respondent
While this may be a version of the truth, AI is still in its nascent stages in many areas of oncology, and its potential to revolutionise cancer care remains immense. And while there are significant challenges facing the widespread adoption of AI in oncology, the potential benefits of this technology cannot be ignored.
Healthcare professionals, patients, researchers, and policymakers must work together to ensure that AI is used responsibly and effectively in oncology and beyond.
"We should try to stay within the conversation around the development of AI tools," Dr. Loaiza-Bonilla advises healthcare professionals. "This way, we'll be on top of issues around ethics, bias, and decision quality."
What excites oncologists about AI?
- I am fearful, not excited. But I’m over 70, so I’m old school!
- The ability to improve clinical research and development of new drugs.
- Standardised care models with high efficacy.
- Personalised treatment plans and predictive analytics.
- Improved earlier diagnosis, and tracking of disease response during radiation therapy.
- The ability to review all available world data on a question about a disease or treatment much faster than you can research it.
- To stay on par with the latest advancements in cancer care.
- Developing predictive tools, and precision medicine to determine if a patient is responding to a treatment, replacement of biopsies and other invasive procedures.
- Identify new trends.
- I am neither excited nor optimistic. I will wait for data to be assessed before embracing any new concept, treatment, or technology.
- Integrating AI with molecular diagnostics (eg, NGS) to identify potential therapeutic targets and match them with targeted therapies.
- Automated thinking and analysis provide physicians with information that is relevant to patient care while avoiding delays in diagnosis, prognosis, and treatment.
Disclaimer: This story is contributed by Tolu Ajiboye and is a part of our Global Content Initiative, where we feature selected stories from our Global network which we believe would be most useful and informative to our doctor members.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries