Obstructive Sleep Apnoea Management
M3 India Newsdesk Nov 06, 2024
Obstructive sleep apnoea, or OSA, is the most common type. It is characterised by repeated episodes of upper-airway obstruction lasting more than 10 seconds during sleep, resulting in pauses in breathing. This article explains the causes and management of OSA especially in paediatric patients.
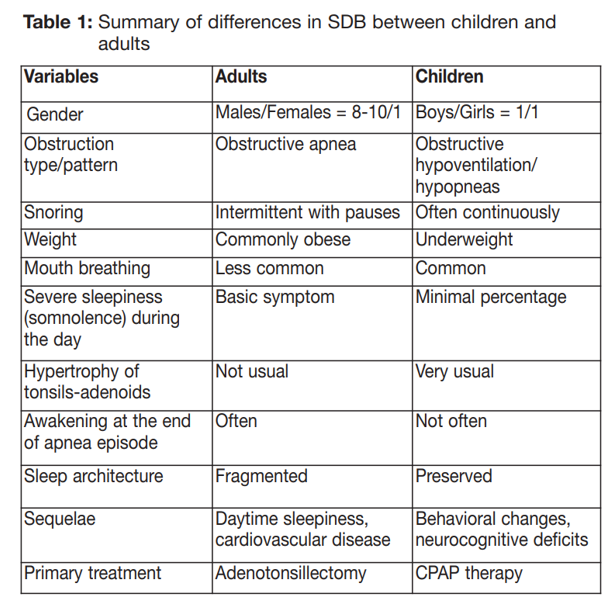
Sleep is a major physiological drive. Children sleep for over half of their lives on average. Breathing disorders during sleep or sleep-disordered breathing (SDB) can cause significant health problems that are associated with high morbidity and a high risk of mortality.
The most widely studied breathing disorders during sleep are obstructive sleep apnoea syndrome (OSA), central hypoventilation and Cheyne-Stokes respiration.
Prevalence of OSA
- Epidemiologic studies have shown that there is a prevalence of about 2% among children and about 2.5%–6% among adolescents.
- OSA in children usually occurs between the ages of 2 and 7 years.
- Initially, though it was thought that both genders were equally affected, it was later observed that boys are more likely to have OSA, which is consistent with the tendency for overweight adult males to have OSA.
Causes
Causes of Obstructive Sleep Apnoea Syndrome in children are discerned as follows:
- Anatomic anomalies, such as hypertrophic tonsils and adenoids (the most common cause in childhood), choanal atresia or stenosis, anomalies of the nasal septum (mainly scoliosis) and soft tissue thickening of the upper respiratory system (polysaccharides, achondroplasia, Prader-Willi syndrome, obesity syndromes).
- Neuromuscular diseases include cerebral palsy, myotonic dystrophy, congenital myopathies, and Arnold-Chiari syndrome. These diseases may coexist with decreased muscle tone in the upper respiratory muscles and defective breathing control by the central nervous system.
- Craniofacial anomalies and syndromes. Most of these conditions coexist with midfacial hypoplasia, micrognathia, hypotony, and sometimes mental retardation.
Management
It is essential to highlight the increased risk factors for OSAS in individuals who are growing, paying particular attention to the aspects associated to dentistry:
- Adenotonsillar hypertrophy (primary cause) is the main issue correlated with OSA in children. Evidence shows that the success rate of an adenotonsillectomy intervention in OSA therapy and resolution is about 83% in children.
- Obesity (especially in adolescence), insulin resistance, hepatic steatosis, and increased production of proinflammatory mediators, that as leptin.
- Nasal resistance can rise and the oropharyngeal space can shrink as a result of abnormalities of the soft tissues (macroglossia) or the maxillary structure (micrognathism and retrognathism). Dentofacial anomalies are frequent in children with OSAS, proving to be a consequence of OSAS, as well as a cause of apnoea itself.
- Neuromuscular disorders, lead to insufficient control of central and peripheral airflow, causing an increased tendency to the collapse of the pharyngeal-hypopharyngeal walls and a muscle tone reduction.
- Obstructive nasal diseases such as asthma or allergic rhinitis, are paediatric determinants of nasal congestion.
- Other factors: age, family history, craniofacial dysmorphism, syndromic diseases (Down syndrome or Pierre Robin sequence), prematurity or multiple pregnancies, and environmental exposure to smoke.
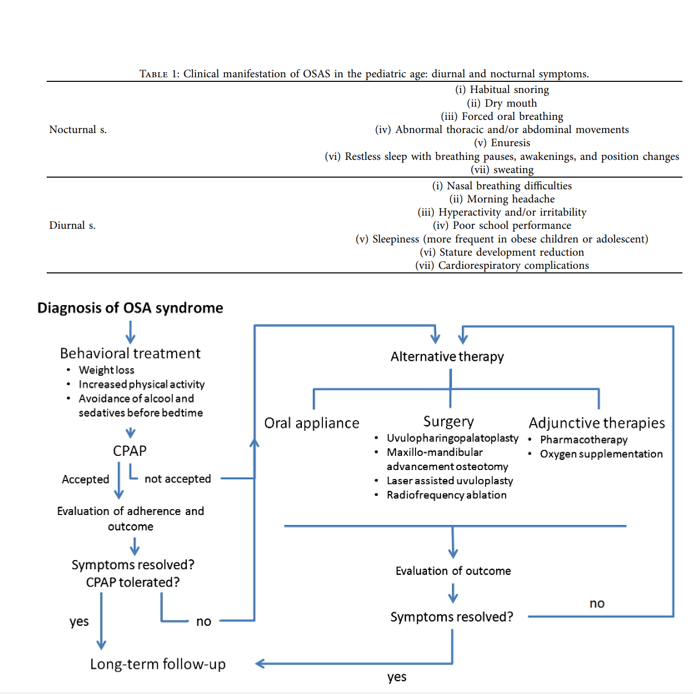
Children with OSAS can currently receive the following symptomatic or causal treatments:
- Lifestyle changes–in particular, weight loss in obese subjects.
- Continuous positive airway pressure (CPAP): While the literature reports CPAP to be the golden standard treatment of OSAS in adults, in the paediatric population, it has been reported as useful only in:
- Patients ineligible for surgery
- Patients awaiting surgery
- Patients with persistent disease after surgery
- Patients with other diseases (i.e., Down syndrome and craniofacial anomalies). It is considered a palliative treatment that causes discomfort in children, who mostly do not get used to it and so become uncooperative
- Pharmacological agents
- Surgery (especially adenotonsillectomy)
- Orthodontic treatments:
- RME (rapid maxillary expansion)
- Myofunctional devices
- Mandibular advancement devices (MADs)

Conclusion
- Paediatric OSA is a serious medical condition and can have long-term consequences on the overall health and quality of life of a patient.
- A dentist should be familiar with the signs and symptoms of OSA and should conduct a thorough history, intra/extra oral examination, and questionnaires and understand the role of comorbid conditions.
- A timely diagnosis and management of OSA can eradicate potential long-term negative effects on the health of a patient.
- If paediatric OSA is suspected a proper referral should be made for the definitive diagnosis and treated accordingly. An interdisciplinary treatment approach may often serve in the best interest of the patient.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Neha Kalantri is a practising dentist from Nashik.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries