Diabetic Diet Plan: A Physician's Perspective by Dr Shilpa Shete
M3 India Newsdesk Dec 30, 2022
The rate of diabetes diagnoses is increasing across the world, including in India. In this article, the author shares her experiences and dietary treatment approaches for diabetes.
Diabetes and lifestyle modification
I frequently come across patients telling me that they do not want to depend on medicines to control their diabetes. Now what can bring the need for medications down is lifestyle modification.
In those who are obese and overweight, lifestyle modification translates into weight reduction. That can work wonders. Nothing else can address diabesity and metabolic syndrome more wholesomely. For those who are in the prediabetic range, lifestyle modification is the only way to step down to non-diabetic status.
Here lies the importance of routine periodic screening. Prediabetes and early/mild diabetes can be entirely asymptomatic, and they are very much reversible by timely and sustained lifestyle changes.
Lifestyle changes need to focus on three interlinked aspects:
- Diet
- Exercise
- Stress management
Goals of diet management in a diabetic patient
- Reduction in fat mass- Total body fat below 30% in women and below 22% in men is considered ideal. In adults over 60 years of age body fat weight targets have been defined as below 35% and below 25% respectively.
- Improvement in muscle mass- Helps improve basal metabolic rate.
- Reducing insulin resistance.
- Minimising vitamin deficiencies.
- Opt for foods/ combinations with lower glycemic index and longer satiety. This helps avoid big peaks and troughs in blood sugar levels and reduces sugar cravings.
- Reduction in Leptin levels thereby reducing chronic systemic inflammation.
Lower waist/hip or fat/muscle ratio translates into lower metabolic age. The gradual and steady loss of body fat and improvement in muscle mass is the key to the reversal of early non-alcoholic fatty liver disease (NAFLD).
Dietary measures for a diabetic/prediabetic person
- Stopping sugar, jaggery, sweets, sweetened beverages, fruit juices and alcohol.
- Lowering carbohydrate intake: including small servings of whole grains (like whole-wheat atta/sooji/ brown rice) instead of refined flour and polished white rice.
- Restricting bakery products.
- Limiting intake of fruits to 2-4 small servings a day. Avoid high glycemic index fruits like bananas, chikoo, grapes, custard apples and mangoes; instead take small servings (1/2 – 3/4 cup) of fruits like apples, pears, berries, oranges, kiwi and melons.
- Increasing intake of proteins in the form of low-fat dairy products, sprouts, fish, egg whites, lean meat and nuts.
- Including large fibre serving in each meal in the form of vegetables and salads.
- Early breakfast, small, high-fibre meals at 3-4 hourly intervals, and dinner before 9 pm (2 hours before bedtime).
Most staple Indian diets are rich in carbohydrates. They provide much less protein than the recommended daily intake of 1gm/kg. It is estimated that irrespective of gender, geographical location and socio-economic status, 85% of Indians lack ideal muscle mass.
Indians are also genetically predisposed to visceral obesity. We are born with more body fat as compared to our western counterparts. Indians with a normal BMI are often found to be ‘fat-thin’. This means that despite having a normal BMI their body fat percentage is above the normal range and muscle mass is less.
Intermittent fasting
We are yet to clearly understand the risks versus benefits of intermittent fasting in those taking medications for type 2 diabetes. Intermittent fasting is not recommended for those with type 1 diabetes. American Diabetes Association does not recommend it as a therapy for type 2 diabetes either.
If a patient taking antidiabetic medications wishes to switch to intermittent fasting, the same should be discussed with the treating physician and nutritionist. Adjustments in medication dosages and timings may be required to suit the new meal timings.
Meals taken during the non-fasting period must be nutrient-dense. Diet needs to be further fine-tuned for every patient keeping parameters like renal profile and liver function in mind. Coexisting (obesity, lifestyle or heredity-related) conditions like hypertension and ischemic heart disease may require additional modifications like reduction in salt intake.
Insulin resistance which is the main culprit in type 2 diabetes causes hyperinsulinemia. Higher insulin levels predispose to the development of hypertension by causing salt retention. Obesity, diabetes and hypertension therefore frequently coexist.
I look forward to discussing these points in more detail in my future write-ups. The benefits of mindful eating shape up only when combined with appropriate exercises, restful sleep and a peaceful mind.
Case study
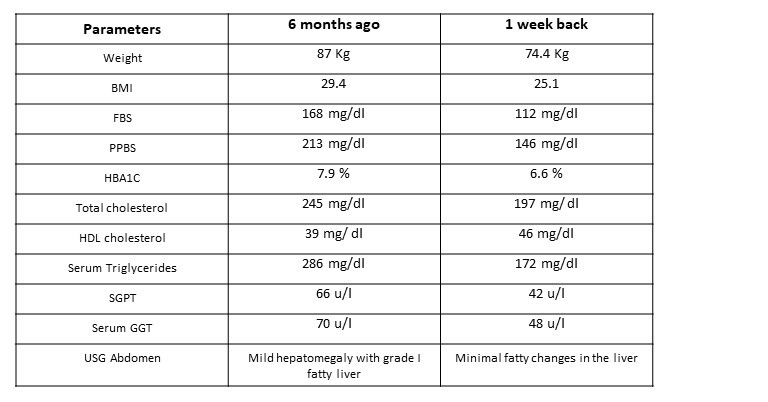
I am glad to share the reports of a 44-year-old male patient I saw 6 months back, and again a week back. He was taking two oral hypoglycemic agents and a statin when I first saw him 6 months back. He led a very busy and stressful work routine and had put on 10 Kg weight over the previous year. He was most willing to change his job and make positive lifestyle changes, which he subsequently did.
I advised him to step up his dose of Metformin and continue the same doses of Sitagliptin and statin. I added fenofibrate, an antioxidant supplement and one multivitamin supplement for 3 months. I explained to him about diet changes that would help him manage his weight, diabetes and overall health in a better way and suggested he follow up with a dietician.
His treadmill test was negative for ischemia so I told him to take up an exercise routine comprising brisk aerobic, stretch and strength training exercises.
His reports are as follows:
Observation
- Some of his parameters are yet to be at goal but he should be reaching there slowly and steadily. He can then be expected to stay there, in all probability with reduced medications.
- He promises to periodically follow up with his dietician and go on with a low-calorie, nutrient-dense diet plan.
- His daily exercise and sleep routine are expected to continue in the same way for another 3 months. He will also be continuing with the same anti-diabetic medications, statin, vitamin D, calcium and vitamin B12 supplements.
Conclusion
I look forward to reviewing his reports after another 3 months and reducing some of his medications. Needless to say, patients following up with such improved reports and improved physical, and mental fitness is an absolute pleasure for any physician. If reports are more than mildly deranged we often do need to step up or add some medications, but it is prudent to encourage and educate patients to simultaneously work on lifestyle modification. Lifestyle modification is the only holistic and sustainable answer to multiple metabolic disorders.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Shilpa Shete is a practising consultant physician from Mumbai.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries