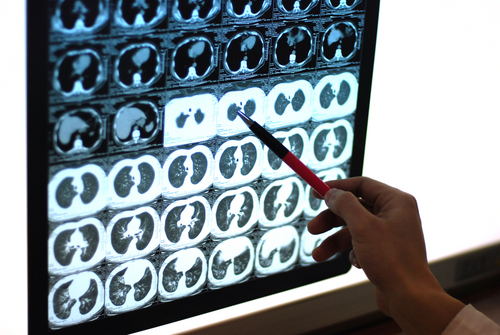
New way to target lung lesions avoids open chest surgery
M3 Global Newsdesk Jan 02, 2019
A new minimally invasive procedure for lung cancer, known as microcoil localization, enables thoracic surgeons to accurately remove small, soft, or deep lung nodules, usually without resorting to open thoracotomy.
With this new method, an implanted wire microcoil directs the surgeon to the precise location of the nodule—reducing time-to-diagnosis, shortening procedure time, and lowering the risk of lobectomy and invasive thoracotomy.
Until recently, surgeons needed to localize lung nodules, as well as ground-glass lung lesions, with direct visualization or digital palpation before resection. This could take extra time and require invasive surgery. Even worse, patients with small lung nodules often had to wait until the lesion grew large enough to be palpated.
“We’re no longer dependent on lesions being palpable to pinpoint their location,” said thoracic surgeon Daniel Raymond, MD, Cleveland Clinic, Cleveland, OH. “Wire localization enables us to localize questionable areas, remove them thoracoscopically, and make a diagnosis.”
Said thoracic radiologist Jason Lempel, MD, also at Cleveland Clinic, “Rather than cutting out an entire lobe, or potentially even an entire lung, we can just take out a small bit of tissue. So, we’re able to treat patients with early-stage lung cancers quickly and thus decrease the chance of the cancer spreading.”
An aggressive approach
The procedure begins with a 22-gauge Chiba needle that’s preloaded with the fiber-coated platinum microcoil, which lies long and straight within the needle’s lumen. The thoracic radiologist uses computed tomography (CT) to guide insertion of the needle into the chest, into the lung, and then into the margin of the target nodule. When the needle tip reaches the nodule, the radiologist pushes out the first part of the elongated microcoil, where it reverts to its natural coil shape—and marks the nodule’s location.
The radiologist then retracts the needle to the pleural surface and deploys the opposite end of the coil into the pleural space before pulling the needle out of the chest. The resulting configuration resembles a dumbbell, with one end of the coil anchored along the nodule, the connecting metallic line in the middle, and the other end of the coil in the pleural space.
Once the coil is in place, the surgeon makes an incision for a video thoracoscope and deflates the lung. Using the thoracoscope, the surgeon locates the coil in the pleural space and then makes a wedge resection that includes the coil and nodule. The lesion is immediately taken to the lab for histopathologic classification.
According to a recent Cleveland Clinic study, led by Dr. Lempel, the preoperative cancer status in 60% of lesions was unknown, but excision clearly established the diagnoses. In the remaining 40% of cases, preoperative diagnoses indicated neoplasms. Overall, 85% of lesions proved to be neoplastic, which, the authors stated, validated the aggressive approach to these small nodules.
“I believe microcoil localization will eventually eliminate the need for lobectomy and conversion to open thoracotomy in many of these situations,” Dr. Lempel said.
No fluoroscopy necessary
The thoracic surgeons at Cleveland Clinic aren’t the only ones currently performing microcoil localization; it was pioneered in North America at Vancouver General Hospital, Vancouver, BC, Canada. However, Dr. Raymond, Dr. Lempel, and thoracic surgeon Sudish Murthy, MD, PhD, added a new twist by accomplishing the procedure without fluoroscopy. Instead, the radiologist tells the surgeon how far the distal end of the microcoil is from the lung’s surface.
“We could use fluoroscopy to confirm that the cut is around the deep end of the coil, but it’s preferable to limit radiation exposure to the patient and surgical staff whenever possible,” Dr. Lempel explains.
A review of the team’s first 20 cases without using fluoroscopy showed a 100% success rate in retrieving the target lesion with clear margins. Further studies with larger numbers of patients are needed to confirm these results, the authors acknowledged.
“CT-guided placement of microcoils is a safe, accurate, and reproducible way of localizing small peripheral pulmonary nodules for VATS [video-assisted thoracic surgery] resection with minimal risk and low complication rates,” they concluded. “With planning, communication, and laboratory follow-up, the present results suggest that intraoperative fluoroscopy is not necessary for successful surgical nodulectomy.”
This story is contributed by John Murphy and is a part of our Global Content Initiative, where we feature selected stories from our Global network which we believe would be most useful and informative to our doctor members.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries