Management of post COVID-19 pulmonary complications: Updated protocols by MoHFW
M3 India Newsdesk May 17, 2022
This part of our article series talks about the effects of COVID infection on the respiratory system in the long term and also elaborates on the spectrum of the problem, its assessment and management guidelines by MoHFW.
The respiratory system is worst hit by viral damage, which may last for many weeks after the initial illness. The nomenclature used to describe the long-term effects of COVID-19 varies considerably. The National Institute of Health and Care Excellence (United Kingdom) created the term "Post-COVID syndrome" to refer to persistent symptoms and signs beyond 12 weeks after the disease start that cannot be attributed to another cause.
Long COVID, according to MoHFW is categorised as Subacute/Ongoing symptomatic COVID: 4-12 weeks and Post-COVID sequelae: signs/symptoms persistent or developing >12 weeks. Additionally, the phrases chronic COVID-19, post-acute COVID-19 sequelae, and long-haul COVID-19 have been used.
A spectrum of the problem
These long-term consequences of COVID-19 may be caused by the virus itself, by broad damage caused by the cytokine storm, by the body's immunological response, by underlying co-morbidities, or by the medicine employed to treat the condition, or by a combination of all of these factors. Following recovery from acute COVID-19 infection, patients may develop widespread lung disease (inflammatory and/or fibrotic), respiratory muscle weakness (most often in patients on mechanical ventilation), pulmonary thromboembolism complications, and pulmonary infections (including mycosis).
At three months following discharge, up to 80% of hospitalised patients with COVID-19 may continue to have breathlessness, however, the incidence of substantial breathlessness (modified Medical Research Council rating 2 or above) is often less than 10%. At three months, computed tomography (CT) of the chest may reveal abnormalities in up to 90% of these individuals. Physiologically, however, a smaller percentage (50-60%) of hospitalised patients would have abnormal lung function tests three months following release.
When do we believe that a patient is suffering from COVID-19's long-term respiratory effects?
Respiratory symptoms and/or delayed or long-term problems of SARS-CoV-2 infection that continue beyond four weeks after the beginning of symptoms should raise concern for sequelae. If no other cause for these respiratory symptoms is identified, the illness is referred to be Long COVID.
The following are the primary symptoms of post-acute COVID-19 respiratory sequelae:
- Breathlessness
- Dry cough
- Chest pain
Certain warning symptoms/signs may be indicative of more significant disorders such as:
- Acute chest pain
- Respiratory distress
- Hypotension
- Hemoptysis
- Fever high grade
- SpO2 less than 90%
- Raised HR / RR
- Cyanosis
- Accessory respiratory muscle use
Initial examination of a patient suspected of having long-term COVID-19 respiratory sequelae
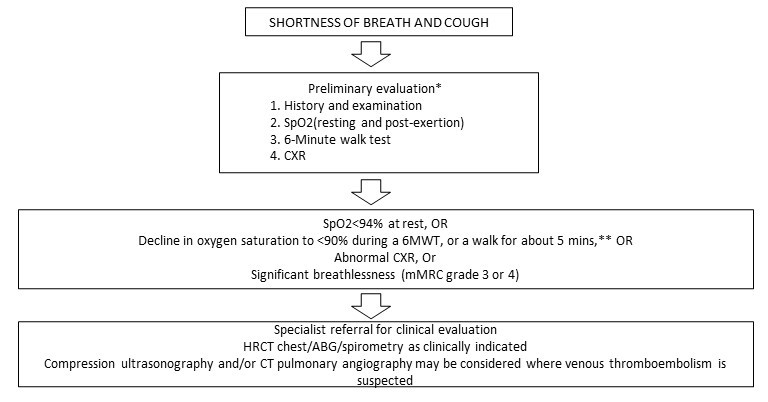
The suggested approach for evaluating individuals who exhibit symptoms consistent with post-COVID respiratory sequelae.
Proposed algorithm for the evaluation of patients with symptoms suggestive of post-COVID respiratory sequelae
Who is at a higher risk for the development of Post-COVID pulmonary sequelae?
There are certain groups of patients who may be at a higher risk for pulmonary sequelae (Box2).
- Elderly >60 yrs
- Smokers
- Comorbid conditions – DM, HT, CAD
- Preexisting respiratory conditions- COPD
- Require O2 at home
- Patients who needed Invasive or noninvasive ventilation during COVID illness
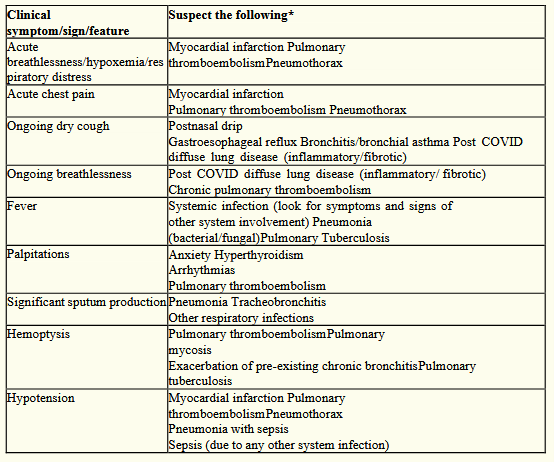
Differential diagnoses for typical cardiorespiratory system symptoms and indicators in the Post-acute COVID phase.
Post-COVID respiratory sequelae patients: What is the first line of treatment?
Post-COVID respiratory sequelae are treated by addressing particular pathologic situations such as Post-COVID diffuse lung disease (PC-DLD), pulmonary embolism, and pulmonary infections. Additionally, it entails the treatment of respiratory problems.
Post-COVID pulmonary problems that need particular management
The therapy for certain pathologic illnesses should be provided by doctors who are knowledgeable about these problems. Below is some guidance.
a) Post-COVID diffuse lung disease- After recovery from an acute COVID-19 infection, residual lung parenchymal abnormalities may signify either chronic inflammatory disease or pulmonary fibrosis. HRCT chest imaging helps determine the amount and nature of such abnormalities. At the moment, there is insufficient solid scientific information to advise therapy of these anomalies.
Observational studies demonstrate that these radiological abnormalities resolve spontaneously in the majority of individuals. Suspected pulmonary fibrosis should be managed by specialists with prior expertise with fibrotic interstitial lung disease.
b) Pulmonary embolism- Patients with pulmonary embolism should get therapeutic anticoagulation. Three months should be the bare minimum length of such therapy. Prolongation beyond this time would be contingent on a risk assessment of recurrence, which must be conducted by a professional. Prophylactic anticoagulation is normally discontinued upon hospital release; however, it may be prolonged as clinically necessary under monitoring.
c) Pulmonary infections- According to established recommendations, secondary bacterial pneumonia should be treated with oral/intravenous antibiotics. Physicians should be aware that the majority of these patients would have had contact with a healthcare institution during the acute COVID-19 sickness, putting them at a greater chance of harbouring resistant bacteria. As cases of pulmonary fungal infection, particularly mucormycosis, have increased in recent years, special attention should be paid to excluding these infections in patients with fever, sputum, and/or hemoptysis. Such infections should be treated in specialised centres with antifungal agents and/or surgical interventions, as indicated.
d) Management of symptoms and general ill-health:
- Healthy diet, regular exercise regimen (suitable for the patient's age and physical condition), and frequent monitoring of critical parameters (like oxygen saturation at rest and during activity, as it is crucial for patients with respiratory sequelae).
- In rare patients, domiciliary oxygen and pulmonary rehabilitation may be necessary.
- Breathing exercises for those with breathlessness or cough. Pharmaceutical interventions may be necessary to control cough and shortness of breath.
- Manage comorbidities adequately
e) Management of cough:
- Coughs should be treated based on their aetiology.
- An appropriate infection assessment should be undertaken in the case of productive cough.
- Simple antitussive medications such as dextromethorphan may be used to treat a dry cough caused by lung disease.
- If the cough is accompanied by wheezing, inhaled bronchodilators (with or without inhaled corticosteroids) may be used.
- Both gastroesophageal reflux and post-nasal drip may be treated with anti-reflux drugs (H2-receptor blockers, proton pump inhibitors, etc.) and antihistaminic agents (with or without antitussives). In the event of an upper airway-related cough, warm saline gargles or lozenges may help calm the throat.
f) Management of breathlessness
- Management may be approached differently depending on the underlying problem.
- Domiciliary oxygen treatment, as described above, aids in the reduction of breathlessness in hypoxemic patients. An organised pulmonary rehabilitation programme aids in the reduction of shortness of breath.
- Patients who are unable to participate in an organised pulmonary rehabilitation programme should be counselled to maintain an appropriate walking regimen for their age and physical condition.
- Caution should be used to prevent overexertion and exercise to the point of hypoxemia.
- Certain breathing techniques may assist alleviate shortness of breath.
Patients should be encouraged to discontinue exercise if any of the following occurs:
- Vomiting or nausea
- Lack of breath
- Vertigo
- Prolonged perspiration
- Chest constriction
- Intensified pain
g) Domiciliary oxygen therapy:
In general, individuals with a resting or exertional oxygen saturation of less than 90% need domiciliary oxygen treatment. It is administered by nasal prongs from an oxygen concentrator or oxygen cylinder.
h) Pulmonary rehabilitation:
A systematic pulmonary rehabilitation programme is recommended for individuals with moderate to severe COVID-19, particularly those who continue to have symptoms beyond the acute episode. Recommendations for individuals with severe COVID-19 with persistent symptoms beyond an acute episode:
- Exercise training and inspiratory muscle activities in a controlled environment.
- Session lasting between 30-45 minutes and scheduled at least 2-3 times per week for a minimum of 8-12 weeks.
- Videoconferencing for monitoring the session if done at home.
The guidelines for post COVID sequel by MoHFW will be discussed in this series pertaining to different organ systems- Cardiovascular, Gastrointestinal, Nephrological, Neurological, and Respiratory. Click here to read the previous parts- Post-COVID cardiovascular sequelae: Latest MoHFW updates, Gastrointestinal symptoms post COVID-19: New MoHFW updates, Post-COVID nephrology related conditions: MoHFW guideline updates,Post-COVID neurological symptoms: MoHFW guidelines for management
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
The author is a practising super specialist from New Delhi.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries