Grave's Disease: How to Manage This Common Thyroid Disorder
M3 India Newsdesk Dec 02, 2022
Grave’s disease is an autoimmune disorder which affects the thyroid gland. The diagnosis and management of this autoimmune disease are elucidated in this article.
Grave's disease
Grave’s disease is the most common cause of thyrotoxicosis. The activating antibody which targets the TSH receptor of the thyroid follicular cells and stimulates thyroid hormone production without normal feedback mechanism results in thyrotoxicosis. It is more common in females (3%) as compared to males (0.5%).
Symptoms like hyperactivity, irritability, altered mood, insomnia, heat intolerance, increase sweating, palpitations, fatigue, weakness, dyspnoea, weight loss, pruritus, thirst, polyuria, oligomenorrhea/ amenorrhoea, loss of libido, erectile dysfunction are similar to hyperthyroidism caused by other causes. The manifestation exclusive to grave’s disease is diffuse goitre, Grave’s ophthalmopathy, localised dermopathy (pretibial myxedema), lymphoid hyperplasia, and thyroid acropachy.

Grave’s dermopathy and Grave’s orbitopathy
Signs associated with grave’s disease are sinus tachycardia, Atrial fibrillation, fine tremor, warm, moist skin, palmar erythema, hair loss, muscle loss and wasting, Congestive heart failure (high output), chorea, periodic paralysis and psychosis. Smoking increases the risk of graves disease and has been associated with the worsening of orbitopathy.
Conditions associated with Grave’s disease are type 1 diabetes mellitus, Addison's disease, vitiligo, pernicious anaemia, alopecia aerate, myasthenia gravis, celiac disease, other autoimmune disorders associated with the HLA-DR3 haplotype.
Diagnosis
Based on the above-mentioned signs and symptoms one can have a high clinical suspicion of Grave’s disease, which is usually seen with diffuse goitre with audible bruit.
Investigation
The thyroid function test is the primary test which shows raised free T4 along with suppression of TSH. As per the guidelines recommendation measurement of TSH-R-Ab is a specific and sensitive tool for rapid and accurate diagnosis and differential diagnosis of Grave’s hyperthyroidism.
Scintigraphy also helps in differentiating the type of thyroid disorder based on the degree and pattern of isotope uptake. In graves, the overall intake of Radioactive iodine uptake is elevated and scintigraphy shows diffuse enlargement of both lobes of the thyroid gland. Ultrasound can also help in differentiating other causes of hyperthyroidism.
Management
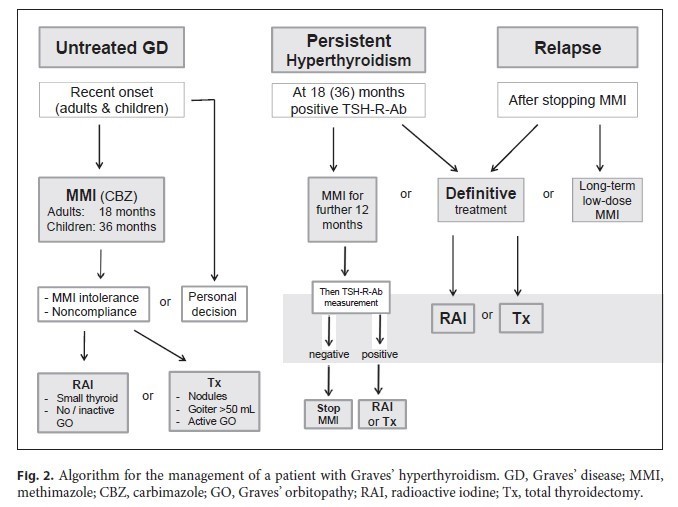
Grave’s disease can be managed by medications, radioiodine iodine (RAI) therapy and thyroid surgery. In the USA the first line of treatment is RAI therapy if there are no contraindications and in Europe, Anti thyroid drugs (ATD) remain the first choice of treatment. As per ETA guidelines the patients should be treated with ATD until the patient prefers RAI therapy or thyroidectomy.
Antithyroid drugs
The aim and principle of medical treatment are to induce remission of Grave’s disease, the patient should be monitored for relapse off treatment, initially 6-8 weeks for 6 months, followed by half yearly for 2 years and then annually thereafter or sooner if the symptoms returns. In cases of relapses consider definitive treatment such as RAI or surgery.
Antithyroid drugs available in the market are carbimazole (CBZ), methimazole and propylthiouracil (PTU). Carbimazole is a prodrug for methimazole. CBZ is the choice of drug in every patient except in the first trimester of pregnancy where the use of CBZ is associated with aplasia cutis or in patients who develops a toxic reaction to CBZ. PTU use is limited by severe liver damage caused by it. Patients should be informed of potential side effects of ATD like agranulocytosis, jaundice, fever, pharyngitis or cystitis.
The typical starting dose of CBZ is 20-30mg/day, higher doses of 40-60mg may be indicated in severe cases. The dose needs titration following a thyroid function test performed every 4-8 weeks. Dose titration should be based on Free T4 levels as TSH may remain suppressed for some weeks after the normalisation of thyroid hormones.
CBZ/MMI is administered for 12-18 months and is to be discontinued once the TSH & TSH-R-Ab are normal. Patients with high TSH-R-Ab levels post-treatment can continue MMI therapy for another 12 months and if it persists to be high, the patient is to be considered for RAI or surgery. Continued long-term low-dose MMI can be considered in patients who are not in remission and who prefer the medical management approach.
Beta-adrenergic antagonists like propanolol should be considered in all suitable patients to relieve symptoms associated with hyperthyroidism like anxiety, tremor and palpitations. The effective dose of propranolol is 20-80mg thrice daily.
RAI therapy
This results in the definitive treatment of relapsed grave disease. The absolute contraindications of RAI are young children, pregnant and lactating mothers, and grave ophthalmopathy, especially in smokers. Conception should be postponed at least 6 months after RAI therapy both in males and females. A dose of 400-800 MBq cures hyperthyroidism in most patients, if thyrotoxicosis persists the dose needs to be repeated only after 6 months. For RAI therapy patients should be referred to an endocrinologist.
Surgery
Total thyroidectomy is considered the procedure of choice because of the risk of relapse with partial thyroidectomy. Surgery is considered in patients with relapse of Grave’s disease, poor compliance to medication, with fear of radiation, and local compressive symptoms due to goitre. Before surgery euthyroidism should be restored to avoid pre and post-operative exacerbation of thyrotoxicosis. In children, thyroidectomy remains the choice of definitive primary treatment. Pregnant women who are not adequately controlled on ATD or who develops serious allergic reaction should be considered for thyroidectomy, performed usually in the second trimester. Lifelong levothyroxine is to be given post-total thyroidectomy.
Conclusion
ATDs are the first-line treatment in Europe, which is given for 18-24 months. ATD helps in remission in many patients with Grave’s disease. RAI is a safe and definitive treatment with a low risk of Grave’s ophthalmopathy progression, particularly seen in smokers. Surgery remains the choice for patients with relapses and indications mentioned earlier. Targeted therapies acting on different steps of the autoimmune process are in preliminary or preclinical stages.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Hitesh Saraogi is a diabetologist and physician at Dhanvantari Hospital, Raj Nagar Extension, Ghaziabad.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries