Malnutrition in Hospitalised Patients: Screening and Management
M3 India Newsdesk Feb 24, 2025
This article reviews current evidence on the diagnosis, clinical impact, and management of hospital malnutrition, considering varying definitions that influence its prevalence and intervention timing.
Malnutrition in hospitalised patients can be screened for and managed using a variety of tools and treatments.
Malnutrition in hospitalised patients heavily affects several clinical outcomes. Malnutrition increases with age, comorbidities, and intensity of care in up to 90% of the elderly population. Thus, an accurate screening to identify individuals at risk of malnutrition or malnourishment is critical for developing a personalised nutritional intervention.
Malnutrition diagnosis necessitates a comprehensive nutritional examination, which is often difficult to do while in the hospital. For this objective, numerous screening procedures were presented, allowing patients to be categorised based on their risk of malnutrition.
Screening tools
Nutritional risk screening is the initial step in identifying at-risk patients and is carried out with simple, quick-to-use tools. It should be implemented methodically and on a regular basis upon admission to a hospital or residential care facility, as well as outpatient for patients with chronic diseases.
Malnutrition Universal Screening Tool (MUST)
A tool that uses weight loss, BMI, and food intake reduction to determine malnutrition risk
Mini Nutritional Assessment (MNA)
A tool that evaluates food intake reduction, mobility, and other factors to determine malnutrition risk
Nutrition Risk Screening 2002 (NRS-2002)
A tool that uses a pre-screening questionnaire to identify patients at risk of malnutrition
Malnutrition Screening Tool (MST)
A tool that uses questions about appetite, nutritional intake, and weight loss to screen for malnutrition
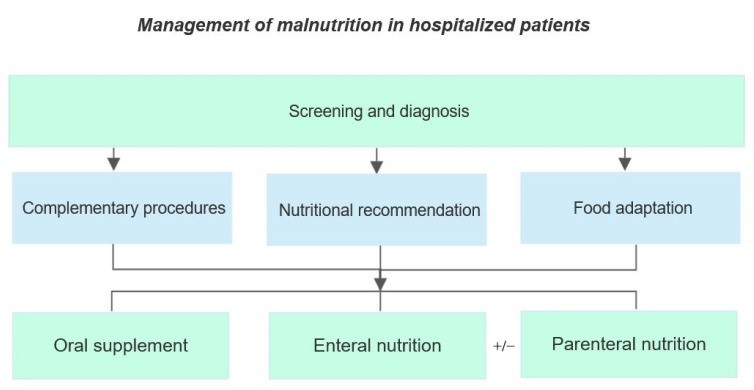
Treatment
- Dietary changes: Eating foods high in energy and nutrients
- Supplements: Taking vitamin and mineral supplements
- Treating underlying conditions: Treating any medical conditions that may be causing malnutrition
- Family support: Helping families manage factors that may affect a child's nutritional intake
- Correcting imbalances: Treating or preventing hypoglycemia, hypothermia, dehydration, and electrolyte imbalance
- Treating infections: Treating or preventing infections
- Feeding: Starting cautious feeding
Malnutrition is often underdiagnosed and undertreated in hospitals. It's recommended to screen all patients for malnutrition risk within the first 24 hours of admission and periodically throughout their stay.
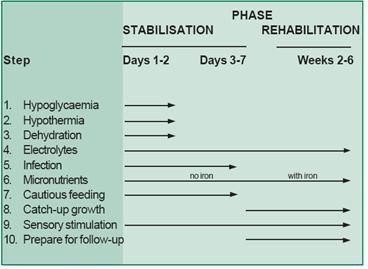
10 steps of routine care
Inpatient treatment takes between 2 to 6 weeks. However, if the appropriate community support is close to where the kid lives, they may be discharged early (at step 8) to continue their treatment at home.
Routine inpatient treatment is summarised in '10 steps’:
1. Treat/ prevent hypoglycemia
Treat hypoglycemia with glucose immediately. To prevent hypoglycemia, feed malnourished children 2-3 hours a day and night. Start straight away.
2. Treat/prevent hypothermia
To treat hypothermia actively re-warm the child. To avoid hypothermia, keep underweight youngsters warm all day and night.
3. Treat/prevent dehydration
Too much fluid can kill. Rehydrate more slowly than usual. Do not give IV fluids except in shock.
4. Correct electrolyte imbalance
Give extra potassium and magnesium daily. Limit sodium (salt).
5. Treat/prevent infection
Antibiotics should be given to all severely malnourished children on a regular basis to treat hidden infections and save lives. Wash hands to prevent cross-infection.
6. Correct micronutrient deficiencies
Provide extra vitamin A, zinc, copper, folic acid, and multivitamins. Do not administer iron until the youngster is in the rehabilitation phase.
7. Start cautious feeding
Give small amounts of F75 every 3 hours day and night. F75 is a specialised formula created to address the demands of malnourished children.
For quick weight gain, give the kid as much F100 or ready-to-use therapeutic food (RUTF) as he or she can consume, eight times per day.F100 and RUTF are rich in calories and protein.
9. Provide sensory stimulation and emotional support
Enhance mental development by offering affectionate attention, play, and excitement.
10. Prepare for follow-up after recovery.
Teach mothers what they can feed their children at home to help them recuperate. Malnourished children require continuous follow-up to prevent relapses and mortality. These steps are accomplished in two phases: an initial stabilisation phase where acute medical conditions are managed, and a longer rehabilitation phase. This is summarised in the table below.
Malnutrition older people
Malnutrition (undernutrition) remains one of the most important health issues for the elderly worldwide. Many causes lead to malnutrition among older persons, including:
- Loss of appetite
- Polypharmacy
- Dementia
- Frailty
- Poor dentition
- Swallowing difficulties
- Social isolation
- Poverty
Malnutrition is common in hospitals, yet it frequently goes unnoticed by medical professionals. This research aims to examine the validity and reliability of Nutritional Screening Tools (NSTs) for older persons in the hospital environment.
This research aims to examine the validity and reliability of Nutritional Screening Tools (NSTs) for older persons in the hospital environment. These include:
- The Subjective Global Assessment (SGA)
- The Mini Nutritional Assessment (MNA)
- The MNA-short form (MNA-SF)
- The Malnutrition Universal Screening Tool (MUST)
- The Simplified Nutritional Appetite Questionnaire (SNAQ)
- The Geriatric Nutrition Risk Index (GNRI)
- Anthropometric measurements
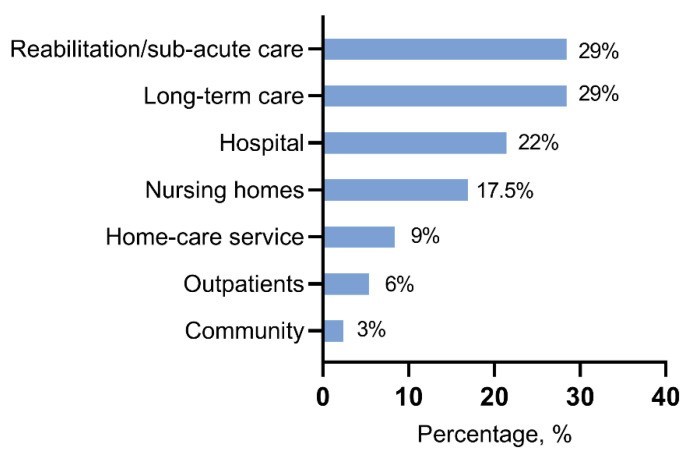
The prevalence and outcomes of malnutrition in hospitalised older adults
- Malnutrition (undernutrition), also known as "hidden hunger," is caused by a variety of conditions, including starvation, sickness, and the ageing process.
- Older persons are more vulnerable to malnutrition, which increases their risk of unfavourable clinical outcomes such as mortality, functional decline, infection, and admission to an aged care facility. Malnutrition in elderly adults in hospitals is highly common, affecting almost half of them. Unfortunately, hospitals have a reputation for contributing to subsequent reductions in nutritional health. Acute illness and injuries might worsen weight loss while hospitalised.
- In addition, there is often an inadequate meal service, with inflexible meal times, limited food choices, insufficient time to eat meals, and a lack of culturally specific food. Meals may also lack sufficient energy requirements for patients, or patients may need to fast before medical tests. Malnutrition is frequently overlooked in hospitals, exacerbating the problem.
- Understandably, early identification of patients with malnutrition in the hospital setting remains crucial for optimal nutritional care. Nutritional Screening Tools (NSTs) are a good way to quickly identify malnutrition. There are a reported 32 NSTs for use in the hospital setting, with 23 of these specific to older adults.
- Despite the great number of screening techniques, the research demonstrates a limited comparison of their validity and reliability for older persons in the hospital context.
- A recent review by Power et al. (2018) looked at the validity of NSTs across various settings, however, they only examined criterion validity (validation against a “gold/reference standard”), and did not investigate construct validity.
- Similarly, a systematic review by van Bokhorst-de van der Schueren and colleagues reported NSTs in the hospital setting, although their results were generic and did not focus specifically on older adults. Another recent systematic review by Marshal et al. The study only examined the validity of nutritional assessment instruments in hospitalised older persons, not NSTs.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Pallavi Dubey has done a Master's in Clinical Nutrition & Dietetics, currently working as a Senior Clinical Nutritionist at Recoup Health, Bangalore.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries