Long Term Health Risks of PCOS
M3 India Newsdesk Sep 06, 2024
This article outlines the health risks of PCOS, including increased chances of diabetes, cardiovascular disease, and cancer, and emphasises the importance of lifestyle management and ongoing monitoring.
Polycystic ovarian syndrome (PCOS) is the most common endocrinopathy among women of reproductive age with an estimated prevalence of about 10%. Type 2 diabetes, cardiovascular disease, endometrial cancer, breast cancer and ovarian cancer are some of the most important emerging issues regarding syndromes' influence on women's future well-being.
Traditionally it is regarded as an endocrine condition presenting with a constellation of symptoms among which anovulation, hyperandrogenism, obesity and acanthosis nigricans are the most common.
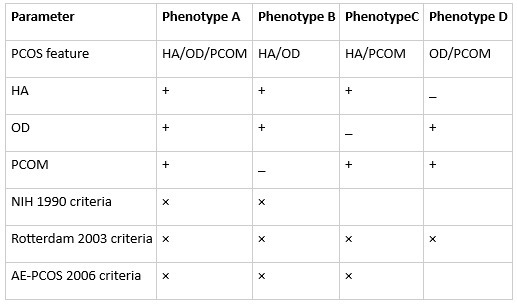
AE-PCOS =Androgen Excess & PCOS Society; HA =hyperandrogenism; NIH = National Institutes of Health; OD = ovulatory dysfunction; PCOM = polycystic ovarian morphology
Classification of PCOS phenotypes
- By the time they are thirty years old, between 25% and 30% of PCOS-affected women will have impaired glucose tolerance, and 8% of these women will become type 2 diabetes each year.
- Angiograms reveal that women with PCOS have more severe coronary artery disease. These women also exhibit hypertension more commonly.
- Endometrial cancer is predisposed in women who experience chronic anovulation, and increasing amounts of data link PCOS to ovarian and breast cancer.
- In Routine clinical practice, it would be helpful to identify those women with PCOS who are at the highest risk for metabolic dysfunction and those with “classic” PCOS phenotypes (phenotypes A and B)
- Epidemiologic research and clinical trials, in which the use of this classification allows researchers to categorise their outcomes on a finite number of PCOS phenotypes, permitting comparisons with other well-defined PCOS populations
Diagnosis
A diagnosis is made when a patient has any two of the following:
- Irregular, infrequent periods or no periods at all
- An increase in facial or body hair and blood tests that show higher testosterone levels than normal
- An ultrasound scan that shows polycystic ovaries.
1. Diabetes
If a patient has PCOS, the patient's risk of developing diabetes is increased further if the patient :
Are over 40 years of age have relatives with diabetes who developed diabetes during pregnancy (known as gestational diabetes), and are obese (a body mass index (BMI) of over 30).
2. Infertility or subfertility
- Many women don't realise they have PCOS until they see a doctor to determine why they cannot get pregnant. Infertility or subfertility (reduced fertility) is a common problem for women with PCOS.
- This may be due to the imbalance of hormones caused by an overproduction of the male hormone testosterone. The ovaries may infrequently release ova (eggs).
3. Metabolic syndrome
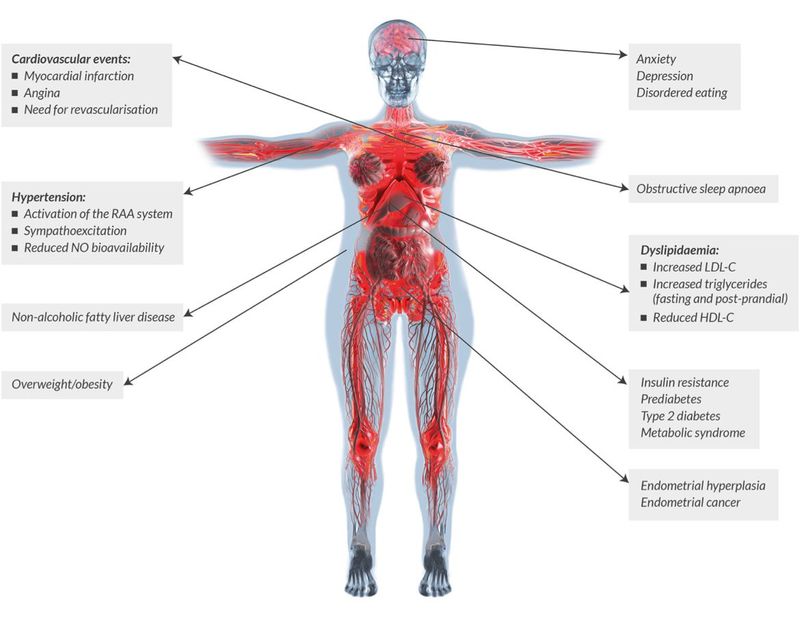
- It is not unexpected that there is a higher risk of metabolic syndrome in PCOS patients, given the condition's links to obesity, insulin resistance, dyslipidemia, and hypertension.
- The risk appears to be more than two-fold more than controls. It is present even after adjustment for age and BMI. As with insulin resistance, PCOS subphenotype may have an important influence, with a greater risk reported in studies in which patients were diagnosed by the NIH rather than Rotterdam or AE-PCOS criteria.
4. Nonalcoholic fatty liver disease (NAFLD)
- NAFLD, or metabolic dysfunction-associated fatty liver disease (MAFLD), is the commonest chronic liver disease in Western societies and is associated with significant morbidity.
- Several risk factors, such as insulin resistance and metabolic syndrome, are shared by PCOS and NAFLD. Insulin resistance raises the lipolysis of adipose tissue, which increases the outflow of fatty acids into the liver and causes hepatic steatosis.
- Owing to these metabolic similarities, a growing body of evidence has recognised an increased risk of NAFLD in women with PCOS. In a large, retrospective longitudinal cohort study in the UK, Kumarendran and colleagues confirmed a 2.2-fold increased risk of NAFLD in young women with PCOS after adjustment for BMI or dysglycaemia.
5. High blood pressure and heart disease
High blood pressure is common in women with PCOS, which is probably caused more by being overweight and insulin-resistant than by the PCOS itself. Treatment for high blood pressure is necessary since it might cause cardiac issues.
6. Cancer
If patients have fewer than three periods a year, the lining of the womb (endometrium) can thicken and this may lead to endometrial cancer in a small number of women.
7. Depression and mood swings
The symptoms of PCOS may affect how patients see themselves and how they think others see them. It can lower a patient's self-esteem.
8. Snoring and daytime drowsiness
Fatigue or drowsiness during the day might be caused by PCOS. It is also associated with snoring.
9. Obstructive sleep apnea
- Studies conducted at the University of Chicago have confirmed the exceptionally high risk of obstructive sleep apnea among women with PCOS.
- Women with PCOS appear to be particularly vulnerable due to causes other than weight, even though it is evident that being overweight increases this risk. For instance, sleep apnea development appears to be influenced by the elevated testosterone levels associated with PCOS.
10. Idiopathic intracranial hypertension (IIH)
- IIH is largely a disease which affects obese reproductive-age women.
- There is an overlap in phenotypic characteristics between PCOS and IIH, and some research indicates that IIH may be more common in PCOS-affected women than in matched controls.
11. Cognitive function
Metabolic risk states such as diabetes and prediabetes are associated with poorer cognition and smaller brain volumes. Researchers have so started to look into whether PCOS exhibits any similar observations, with varying degrees of success.
Prevention
Advice healthy lifestyle
The primary strategies for lowering the total risk of chronic health issues include:
- Eating a healthy balanced diet. This should include fruit and vegetables and whole foods (such as wholemeal bread, whole-grain cereals, brown rice and whole-wheat pasta), cut down the amount of sugar, salt and caffeine.
- Eating meals regularly, especially breakfast.
- Engage in moderate exercise three times a week for at least thirty minutes.
- Advise regular health checks.
- It should aim to keep weight at a normal level. BMI between 19 and 25.
- If patients are overweight, it would be helpful to lose weight and maintain weight at this new level.
The benefits of losing weight include:
- A lower risk of insulin resistance and developing diabetes
- A lower risk of heart problems
- Lower risk of cancer in the womb
- More regular periods
- An increased chance of becoming pregnant
- a gradual decrease in both acne and overgrowth of hair
- Improved mood and self-esteem
Patients only have to lose a small amount of weight to make a difference in their symptoms and their health. Women with a BMI over 40 may consider weight loss surgery.
Because PCOS carries several long-term health hazards, it is imperative that women who are "at risk" have a lifelong follow-up to identify and promptly avoid issues.
Conclusion
- Women with PCOS who also have subclinical vascular disease, obesity, dyslipidemia, hypertension, cigarette smoking, and impaired glucose tolerance are at risk for CVD, whereas those who have metabolic syndrome and/or type 2 diabetes mellitus are at high risk.
- Measurements of body mass index, waist circumference, blood pressure, serum lipid/glucose, and oral glucose tolerance tests are advised for all women with PCOS, as well as for those who are obese, elderly, have a personal history of gestational diabetes, or have a family history of type 2 diabetes mellitus.
- Mood disorder assessment is suggested in all PCOS patients.
- Lifestyle management is recommended for primary CVD prevention, targeting low-density and non-high-density lipoprotein cholesterol and adding insulin-sensitising and other drugs if dyslipidemia or other risk factors persist.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Sejal T Modi, MD, DGO practising in Mothers maternity and nursing home, Ahmedabad.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries