Leprosy: Let Us Learn More About This Ancient Disease
M3 India Newsdesk Jan 29, 2023
Leprosy is a chronic infectious disease involving a culmination of myriad signs and symptoms as multiple systems are involved. The classification, causes, clinical manifestations and treatment of leprosy along with its prevention are discussed in this article.
Leprosy (Hansen’s disease)
Leprosy is also known as Hansen’s disease after Norwegian scientist Gerhard Henrik Armauer Hansen. The causative bacteria may take years to grow once affected and hence this condition is considered slow and progressive in nature.
Causative organism: Mycobacterium Leprae
Classification of leprosy
WHO classification
- Single Lesion Paucibacillary (SLPB) -These patients have a single skin lesion and no other sign.
- Paucibacillary (PB) leprosy -This includes the following types in the Ridley-Jopling classification:
- Indeterminate (I)
- Polar tuberculoid (TT)
- Borderline tuberculoid (BT)
- Multibacillary (MB) leprosy-This term refers to patients with 6 or more skin lesions, and a positive slit skin smear (if obtained). It includes the following subtypes of the Ridley-Jopling classification:
- Polar lepromatous (LL)
- Borderline lepromatous (BL)
- Mid-borderline (BB) is defined as having 6 or more skin lesions and a positive skin smear if available
Mechanism of action
The M. Leprae bacteria mainly affects the peripheral nervous system and the skin but is also seen to affect the eyes, bones, mucous membrane, testes and this produces various clinical manifestations.
1. Peripheral nervous system
In the peripheral nervous system, the M. leprae bacterium is found in to the Schwann cells. Once inside the host cell, M. leprae interacts with the host cell’s lipid metabolism to foster bacterial intracellular survival and this triggers the cells to de-differentiate into immature cells through the activation of signalling of the Erk1/2 pathway. This de-differentiation leads to the reprogramming of the Schwann cells to a “stem cell-like” cell which now has capabilities, like re-differentiation into mesenchymal cells with the ability to spread infection or attract macrophages to develop granulomas that could lead to systemic dissemination of M. leprae.
2. Skin
In the skin, M.leprae is found in keratinocytes, histiocytes and macrophages. Keratinocytes lead to the release of the antimicrobial peptide β-defensin in response to M.leprae antigens.
Transmission
Leprosy is transmitted via droplets, from the nose and mouth, during close and frequent contact with the affected patients
Epidemiological data
- 127558 new leprosy cases were detected globally in 2020, according to official figures from 139 countries from the 6 WHO Regions, including 8629 children below 15 years.
- The new case detection rate the among child population was recorded at 4.4 per million child population.
- At the end of the year 2020, the prevalence was 129 389 cases on treatment and the prevalence rate corresponds to 16.7 per million population.
- The countries with the highest number of new leprosy diagnoses every year are India, Brazil, Indonesia and Bangladesh with more than half of all new cases of leprosy diagnosed in India.
- In 2020 65,147 (51 %) new cases of leprosy were found there (this number is much lower than usual due to the challenges to diagnosing and treating new cases posed due to the COVID-19 pandemic).
- In 2020,15 countries reported more than 1,000 new cases of leprosy, which were Bangladesh, Brazil, DR Congo, Ethiopia, India, Indonesia, Madagascar, Mozambique, Myanmar, Nepal, Nigeria, Philippines, Somalia, Sri Lanka, Tanzania.
Clinical manifestations
1. Peripheral nervous system
The presence of M.leprae at this site produces nerve infection, axonal dysfunction and demyelination leading to sensory loss accompanied by associated disability and deformity.
Symptoms are as follows:
- Numbness of the affected area of the skin
- Muscle weakness
- Paralysis of the affected part
- Enlarged nerves of the affected part
- Vision problems due the damage to the facial nerve
- Acute Neuritis
- Silent nerve paralysis
- Sub-clinical neuropathy
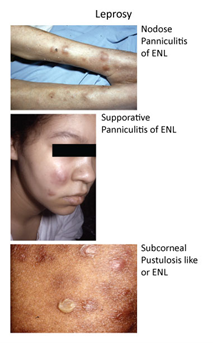
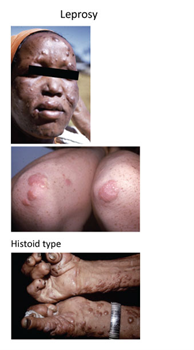
2. Skin
- Discoloured patches of the skin are usually flat and sometimes numb too. The appearance of the patches is usually lighter than the skin around them.
- Thick and dry skin.
- Nodular growths on the skin.
- Loss of eyelashes and eyebrows.
- Painless ulcers on the foot.
- Painless swellings or lumps on the face and earlobes.
3. Mucous membrane
- Nose bleeds
- Stuffy nose
4. Signs of untreated advanced leprosy
- Shortening of toes and fingers
- Paralysis and crippling of hands and feet
- Chronic non-healing ulcers on the bottom of the feet
- Blindness
Diagnosis
According to the recent guidelines of the WHO, there are no additional tests required other than considering one of these three cardinal signs:
- Definite loss of sensation in the pale and hypopigmented area or the same symptom in the reddish patch.
- Enlarged peripheral nerves with loss of sensation and weakness of the muscles supplied by the affected nerve.
- Presence of acid-fast bacilli in a slit-skin smear.
Supplementary clinical diagnostic tests
- Enzyme-linked immunosorbent assays (ELISA)
- Polymerase chain reaction (PCR)-based assays
- Lateral flow assays
However, these tests lack an accurate clinical diagnostic value and are not very reliable and can just be used as a adjunct. According to the recent guidelines no diagnostic testing should be done in case of asymptomatic contacts because the the accuracy of diagnosis in such cases is very low and unreliable.
Differential diagnosis
- Superficial fungal infections
- Psoriasis
- Seborrhoeic dermatitis
- Lupus erythematosus
- Lupus vulgaris
- Acute inflammatory disorders of the skin
- Macular syphilides
- Leishmaniasis
- Post-inflammatory hypopigmentation
- Neurofibromatosis
Treatment
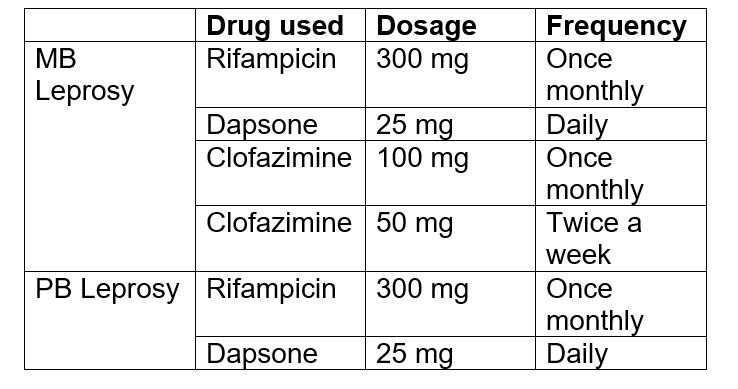
Regimen for adults
 Regimen for children (less than 10 years of age)
Regimen for children (less than 10 years of age)
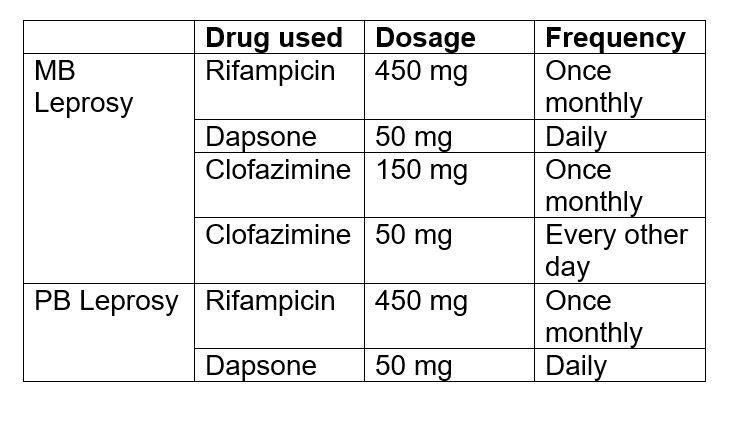
 Regimen for children (between 10-14 years of age)
Regimen for children (between 10-14 years of age)
Social stigma and mental health impairment
Studies show that mental health suffering, depression and anxiety were triggered in patients suffering from leprosy due to isolation by families, friends and society. The presence of deformities creates a sense of fear and embarrassment in patients due to societal stigma and associated prejudice.
Prevention
- A multidisciplinary approach towards the prevention of leprosy aims towards preventive rehabilitation in order to help people avoid disability due to the condition. This consists of the prevention of disabilities by an early diagnosis and prompt treatment.
- Conduct health awareness campaigns for creating more awareness and increase knowledge among the subjects, especially in endemic areas.
- Improving healthcare coverage and increasing access to dedicated healthcare for the marginalized population.
- To train more healthcare staff to improvise the detection and treatment of leprosy.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Ridima Surve (FL) is a practitioner from Mumbai.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries