Irritable Bowel Syndrome Management: Understanding FODMAPs
M3 India Newsdesk Oct 15, 2024
Irritable Bowel Syndrome (IBS) is a functional gastrointestinal disorder affecting approximately 10-15% of the global population, with a higher prevalence in women. This article discusses the pathophysiology of IBS and the role of diet in its management along with some case studies.
Introduction
Irritable Bowel Syndrome (IBS) is characterised by chronic abdominal pain, bloating, and altered bowel habits, including diarrhoea, constipation, or a combination of both. Despite its high prevalence, the exact etiology of IBS remains unclear, and management strategies focus on symptom relief. Dietary intervention is a cornerstone in the management of IBS, with the low-FODMAP diet emerging as a key therapeutic strategy.
Pathophysiology of IBS
The pathophysiology of IBS is complex, involving interactions between the gut-brain axis, gastrointestinal motility disorders, visceral hypersensitivity, and gut microbiota alterations. Stress and psychological factors can exacerbate symptoms, while dietary triggers, such as certain carbohydrates, fats, and fibers, can lead to symptom flare-ups. IBS is now understood as a biopsychosocial disorder, where diet plays a crucial role in symptom modulation.
The role of diet in IBS management
For many IBS patients, food intake directly correlates with symptom severity. Common dietary triggers include caffeine, alcohol, spicy foods, and high-fat meals. However, managing IBS often requires more than just avoiding these general triggers. Personalised dietary interventions, especially those focused on fermentable carbohydrates, can significantly improve patient outcomes.
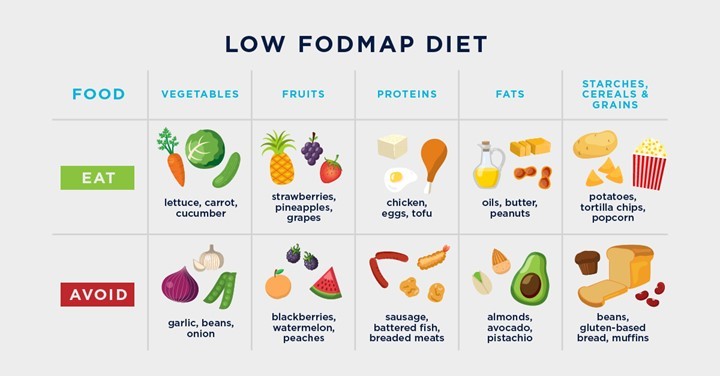
The low-FODMAP diet, developed by researchers at Monash University, is currently the most effective dietary approach for managing IBS symptoms. It involves reducing the intake of certain fermentable carbohydrates that are poorly absorbed in the small intestine, leading to symptoms like bloating, diarrhoea, and abdominal discomfort.
Understanding FODMAPs
FODMAPs (Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols) are short-chain carbohydrates that are poorly absorbed in the small intestine. Few examples of high FODMAP foods are:
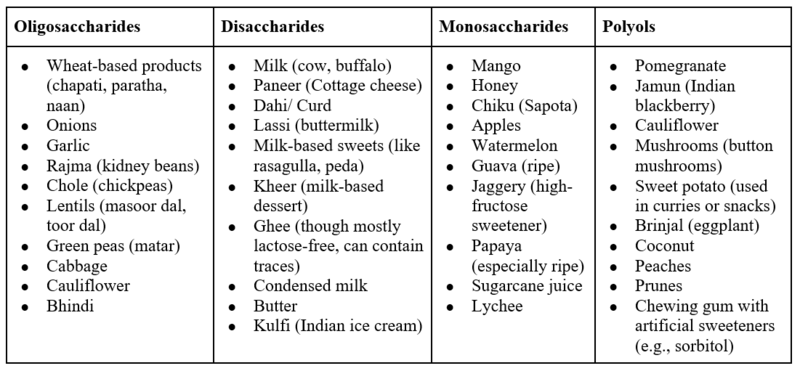
These carbohydrates are not fully broken down in the small intestine and, as a result, are fermented by gut bacteria, leading to gas production, bloating, and altered bowel movements. The low-FODMAP diet aims to reduce these symptoms by eliminating foods high in FODMAPs and gradually reintroducing them to determine individual tolerances.

Implementing the low-FODMAP diet in clinical practice
The low-FODMAP diet consists of three phases:
- Elimination phase: A strict avoidance of all high-FODMAP foods for 4-6 weeks. This phase is crucial for identifying symptom relief and ensuring the patient can differentiate between food-induced symptoms and those from other triggers.
- Reintroduction phase: Gradual reintroduction of individual FODMAP groups to determine specific triggers. This phase helps personalise the diet and identifies which FODMAPs the patient can tolerate in small quantities.
- Personalisation phase: A tailored long-term diet plan that allows the patient to enjoy a variety of foods without triggering symptoms. The goal is to minimise restrictions while maintaining symptom control.
Efficacy of the Low-FODMAP diet
- Several randomised controlled trials have demonstrated the efficacy of the low-FODMAP diet in reducing IBS symptoms, particularly in terms of abdominal pain, bloating, and stool consistency.
- A study by Staudacher et al. (2017) showed that approximately 70% of IBS patients experienced significant symptom relief following a low-FODMAP diet.
- Research from Monash University has also contributed significantly to this field, providing evidence that this dietary approach can lead to long-term symptom control in most patients.
- However, while the low-FODMAP diet is effective, it can also be nutritionally restrictive if not properly monitored.
- There is a risk of micronutrient deficiencies if the diet is followed for an extended period without the guidance of a healthcare professional, particularly a dietitian.
Considerations for long-term management
The low-FODMAP diet is not intended to be a lifelong solution. Once symptom control is achieved, healthcare professionals should work with patients to liberalise their diet as much as possible.
Personalised approaches that incorporate stress management, lifestyle modification, and psychological support should complement dietary therapy. Additionally, fiber intake, hydration, and regular physical activity should be emphasised to promote overall gastrointestinal health.
Case studies
Case study 1
A 32-year-old female with IBS-D (Diarrhoea predominant)
This patient presented with chronic diarrhoea, bloating, and cramping for over two years. After initiating the low-FODMAP diet, she experienced significant relief within four weeks. During the reintroduction phase, it was discovered that fructose and lactose were her primary triggers. Her long-term management now includes a low-fructose and lactose-free diet, resulting in a significant improvement in her quality of life.
Case study 2
A 45-year-old male with IBS-C (Constipation predominant)
The patient had a history of chronic constipation, abdominal pain, and significant bloating. After four weeks on the low-FODMAP diet, his bloating and discomfort were alleviated. The reintroduction phase identified polyols and fructans as his primary triggers. He was able to reintroduce some oligosaccharides without symptoms and now maintains a modified low-FODMAP diet that includes fiber-rich, non-fermentable foods to promote regular bowel movements.
Case study 3
A 28-year-old female with IBS-M (Mixed diarrhoea and constipation)
This patient had alternating diarrhoea and constipation with bloating and gas. The low-FODMAP diet provided symptom relief within three weeks. Through the reintroduction phase, it was determined that oligosaccharides and polyols were the main triggers. Her current management includes a diet low in these FODMAP groups, alongside mindfulness practices to manage stress, which she identified as a key exacerbating factor.
Conclusion
Dietary management, particularly the low-FODMAP diet, plays a central role in the management of IBS. The elimination and reintroduction process provides a structured approach to identify individual triggers while improving overall symptom control. However, long-term adherence to the diet should be personalised and guided by healthcare professionals to prevent nutritional deficiencies. By integrating diet with other lifestyle modifications, the management of IBS can be greatly optimised, improving patient quality of life.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
The author of this article: Ms Rutambhara Nhawkar is a Clinical Dietician, M. Sc. (Clinical Nutrition & Dietetics), Certified Diabetes Educator and a medical writer from Pune.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries