Innovative Oncology: 5 Current and Upcoming Therapies Changing the Game
M3 Global Newsdesk Sep 02, 2023
In recent years, the field of oncology has witnessed remarkable advances in the development and use of novel, game-changing therapies. These revolutionary treatments offer more targeted and personalised approaches to cancer management, paving the way for significant improvements in patient outcomes.
In this special report, MDLinx interviewed a group of oncologists to identify and shine a spotlight on five of these game-changing modalities, and to explain how and why they are so crucial to today's patient outcomes.
They also identified two “future changers” that have the potential to impact treatment choices for years to come.
Each treatment has brought about a paradigm shift in how cancer is treated, whether it’s by overcoming resistance mechanisms, leveraging individual patients' unique disease characteristics, or harnessing the patient's immune system to fight malignancies more effectively.
Antibody-drug conjugates
Antibody-drug conjugates (ADCs) are targeted cancer treatments that work by combining a cancer-killing drug with a specific antibody.
“ADCs provide a way to focus the effects of the chemotherapy drug where it's most needed—in the cancer itself.”
— Jeffrey Bubis, DO, FACOI
The antibody seeks out cancer cells, binds to them, and delivers the drug directly to the cancer cells. This destroys the cancer cells while minimising collateral damage to healthy cells.
Since the first FDA approval in 2000, ADCs have significantly changed oncology treatments.
“ADCs provide a way to focus the effects of the chemotherapy drug where it's most needed—in cancer itself,” explained Jeffrey Bubis, DO, FACOI, Division Director and Attending Hematologist/Medical Oncologist at Florida Cancer Specialists & Research Institute in Fleming Island, FL. “It's a novel option for treating some cancers, like breast and lung cancers, with acceptable toxicity levels.”
ADCs offer a therapeutic alternative for cancers with poor prognoses and limited treatment options. In fact, they are one of the fastest-growing oncology drug classes. As of 2022, fourteen ADC drugs had received approval for solid and haematological cancers.
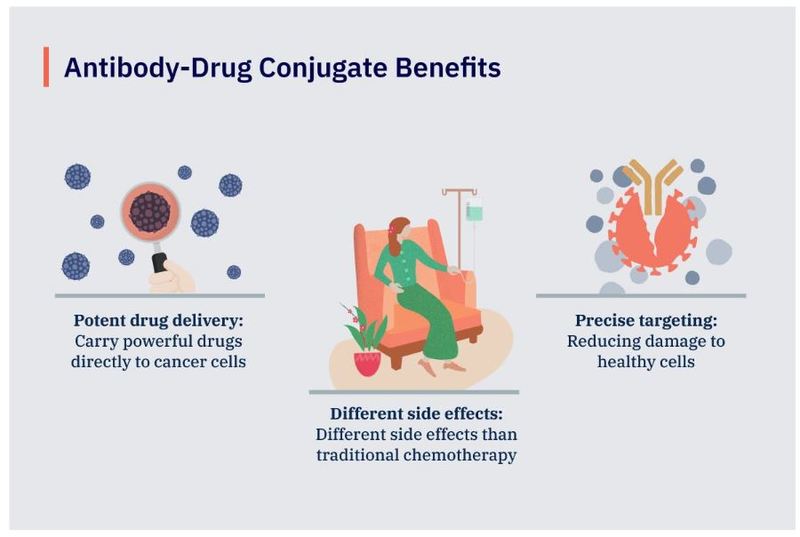
Advantages of ADCs
Some of their major advantages include:
- Potent drug delivery: ADCs can carry powerful drugs directly to cancer cells, increasing their effectiveness in killing cancer cells.
- More precise targeting: ADCs selectively target cancer cells, improving treatment specificity and efficacy, minimising systemic drug distribution, and consequently reducing damage to healthy cells.
- Different side effects: By sparing healthy cells, ADCs generally cause different side effects than traditional chemotherapies do.
“In the case of breast cancer specifically, an ADC can improve overall survival,” Dr Bubis added. “ADCs have rapidly become a standard of care.”
Neoadjuvant and adjuvant immunotherapy in early-stage NSCLC
While immunotherapy for NSCLC has been around long enough to become a standard of care, it’s the timing of the administration that is giving the therapy a second chance at game-changing status.
Cancer immunotherapy works by boosting the body's immune system to help it fight, control, or prevent cancer. Neoadjuvant immunotherapy is administered before surgery in early-stage non-small cell lung cancer (NSCLC) to shrink tumours and make surgery more effective.
Adjuvant immunotherapy, on the other hand, is given after surgery to eliminate any remaining cancer cells and to reduce the risk of recurrence.
“For a long time, we essentially had no therapies for stage 2/3 NSCLCs except for the archaic platinum combos, which are hard to tolerate and present high relapses.”
— Darshan Gandhi, MD, MBA
“For a long time, we essentially had no therapies for stage 2/3 NSCLCs except for the archaic platinum combos, which are hard to tolerate and present high relapses,” says Darshan Gandhi, MD, MBA, medical oncologist at Texas Oncology–Methodist Charlton Cancer Center in Dallas, TX. “It all started with durvalumab maintenance in locally advanced NSCLC, which showed improvement in PFS for the first time. Now we see ICIs [immune checkpoint inhibitors] moving further up the line in the neoadjuvant setting.”
Currently, the primary use of neoadjuvant and adjuvant immunotherapy for early-stage NSCLC is in combination with chemotherapy.
According to the CDC, lung cancer is the third most common cancer in the United States, and more people die from it than any other type of cancer. Over the past decade, the number of diagnoses of early-stage lung cancer has gradually increased as lung cancer screening becomes more commonplace.
Given that immunotherapy with ICIs has been established as revolutionary in the treatment of advanced NSCLC, there is rising interest and enthusiasm for the role it could play in treating early-stage NSCLC.
“I believe this will dramatically change the early-stage paradigm as multidisciplinary tumour boards begin to discuss neoadjuvant approaches upfront, prior to patients going to the operating room for lobectomies,” Dr Gandhi added.
In March 2022, the ICI nivolumab combined with platinum-doublet chemotherapy became the first FDA-approved neoadjuvant treatment for adult patients with resectable NSCLC.
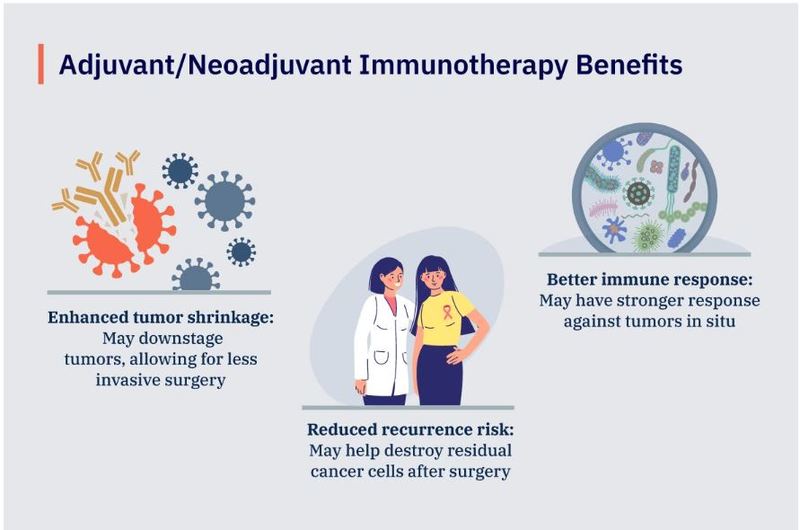
Using neoadjuvant and adjuvant immunotherapy in early-stage NSCLC appears to offer immense benefits by harnessing the patient's immune system to fight cancer more effectively. Additional benefits include:
- Enhanced tumour shrinkage: Neoadjuvant immunotherapy can shrink tumours significantly, potentially downstaging tumours and making surgery more successful and less invasive.
- Reduced recurrence risk: Adjuvant immunotherapy helps destroy residual cancer cells after surgery, lowering the risk of recurrence.
- Better immune response: Research on neoadjuvant immunotherapy suggests that immunotherapy induces a stronger response against the tumour if it is administered while the tumour is in situ, rather than after it's been surgically removed.
“The bar for adjuvant therapies is always a bit higher, as we prefer to see improvement in overall survival, which does take time to show statistically,” Dr. Gandhi said. “Typically, we like to see improvement in pathological response rates for neoadjuvant therapies. However, the expectation is that it will translate into an OS benefit in the long run. We have several ongoing trials looking at these outcome endpoints, and I personally think these will become standard of care over the next 3 to 5 years.”
Adjuvant CDK4/6 inhibition in high risk, HR+/HER2– breast cancer
CDK4/6 inhibitors are a class of drugs that target and block the activity of cyclin-dependent kinases 4 and 6. These kinases play a crucial role in cell cycle regulation. By inhibiting CDK4/6, this modality prevents cancer cells from proliferating uncontrollably—eventually slowing down or stopping tumour progression. CDK4/6 inhibitors are typically used in combination with hormone therapy to treat HR+/HER2– breast cancer.
“The addition of CDK4/6 inhibitors [specifically, palbociclib, abemaciclib, and ribociclib] to endocrine therapy [ET] has improved progression-free survival significantly in metastatic disease,” according to Erica Linden, MD, Medical Director of Breast Oncology and Cancer Genetics at Capital Health in Pennington, NJ. “They have extended the time until needing new therapies to more than 25 months on average—and in many patients for years—compared to 14.5 months with ET alone.”
Currently, CDK4/6 inhibitors in combination with hormone therapy (aromatase inhibitor or fulvestrant) are FDA-approved for first- or second-line treatment of patients with HR+/HER2– or metastatic breast cancer.
“Once we had established that CDK4/6 inhibitors were effective in metastatic/advanced breast cancer, the question was whether this would help patients at high-risk for recurrence with localised disease.”
— Erica Linden, MD
HR+/HER2– is the most common breast cancer subtype, and more than two-thirds (70%) of early breast cancers are diagnosed as HR+/HER2– . The three approved CDK4/6 inhibitors have revolutionised the treatment of metastatic HR+/HER2– breast cancer.
Moreover, while adjuvant ET significantly reduces the risk of recurrence and death among patients with HR+/HER2– early breast cancer, as many as 20% of patients will still experience recurrences in the first 10 years. Because of this, researchers seek to expand their use in combination with ET in the adjuvant setting. While research and clinical trials are ongoing, a few meta-analyses have shown beneficial results.
Based on those results, the FDA approved the use of the CDK4/6 inhibitor abemaciclib in combination with ET for adjuvant treatment of patients with HR+/HER2– early breast cancer at high risk of recurrence.
This initial approval in 2021 limited the use of this adjuvant therapy to this high-risk population, with the added requirement of having a Ki-67 score ≥20%. More recently, however, the FDA removed the additional Ki-67 score requirement.
"Once we had established that CDK4/6 inhibitors were effective in metastatic/advanced breast cancer, the question was whether this would help patients at high-risk for recurrence with localised disease," said Dr Linden. "The MonarchE trial established that the use of adjuvant abemaciclib reduced the risk of recurrent disease in patients at high risk for recurrence. These medications have become the standard of care in adjuvant therapy. "
Additional phase 3 data on the CDK4/6 inhibitor ribociclib is anticipated at the upcoming ASCO conference in June.
Bispecific antibodies
Bispecific antibodies are special proteins designed to stick to two different targets at once.
They bind to a specific antigen on cancer cells and to a receptor on immune cells, such as T-cells. This connection brings the immune cells close to the cancer cells, improving the immune system's ability to recognise and kill cancer cells more effectively.
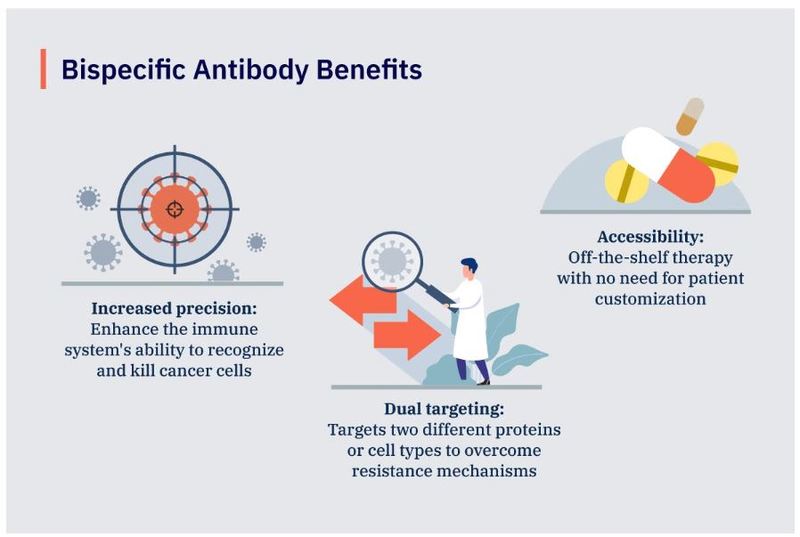
Benefits of bispecific antibodies
Bispecific antibodies are a type of immunotherapy that offer several benefits and fill important gaps in medical oncology:
- Increased precision: By connecting cancer cells to immune cells, bispecific antibodies enhance the immune system's ability to recognise and kill cancer cells specifically, reducing damage to healthy cells.
- Dual targeting: Naturally occurring antibodies and standard antibody drugs typically only target one antigen. The ability to target two different proteins or cell types at once increases treatment effectiveness and can overcome resistance mechanisms.
- Accessibility: Bispecific antibodies are an alternative to CAR-T cell therapies—a cellular therapy that is not approved in all cancers. While both therapies work in a similar fashion, bispecific antibodies are off-the-shelf therapies with no need for customisation, whereas CAR-T cell therapy currently requires personalised engineering of each patient's T-cells.
Bispecific antibodies also have lower treatment complexity. The first few doses are given in a hospital setting, but subsequent doses can be administered as injections in community-care settings. CAR-T cell therapy involves a more complex process and can only be administered in an inpatient setting.
“Bispecifics are the most recent therapy to market for which we have the shortest follow-up data,” according to Dr. Bubis. “But they offer a lot of potential, particularly for patients with multiple myeloma and lymphomas. They are a late-line treatment that can help bridge patients for transplants and potentially extend the life of those who have exhausted all other options."
Nanoparticle technology for glioblastoma
Nanoparticle (NP) medical technology uses tiny particles, typically ranging from 1 to 100 nm in size, for various therapeutic and diagnostic applications. These nanoparticles can be made from multiple materials, including lipids, polymers, metals, and other organic or inorganic compounds.
NP-based drug delivery systems in cancer treatment have shown many advantages, such as good pharmacokinetics, precise tumour cell targeting, and reduced side effects and drug resistance. They are, however, quite novel in the treatment of glioblastomas.
Glioblastoma (GBM) is the most common and most aggressive type of brain malignancy, accounting for 14.5% of all CNS tumours and 48.6% of malignant CNS tumours in the United States.
Patient outcomes are abysmal—the median survival is less than 15 months with the current standard of care, which involves surgery followed by radiotherapy and chemotherapy.
Existing immunotherapies, which have revolutionised treatment for many cancer types, are less effective in treating glioblastomas. One primary reason for this is that the tumour microenvironment is hostile to immune response due to the presence of many immune-suppressive mechanisms.
Researchers and scientists are currently developing ways to overcome these limitations by using nanoparticles to deliver anti-cancer therapy directly to glioblastomas. While most are still investigational, NanoTherm™, a nanoparticle formulation indicated for treating primary or recurrent glioblastoma multiforme, has been approved by both the FDA and the European Medicines Agency (EMA).
Looking back toward the future
Game-changers can only change the game for so long.
To keep the wheels of progress moving, researchers constantly need to find new ways to attack tumours and improve patient outcomes. While that certainly does include the continued identification of novel molecules and pathways, breakthroughs can also be found in extant therapies.
NCI match trial
The NCI-MATCH Trial (Molecular Analysis for Therapy Choice) is a groundbreaking precision medicine study initiated by the National Cancer Institute (NCI). The goal of the trial was to determine whether treating advanced or rare cancers based on an individual patient’s specific genetic mutations would be viable.
At its inception, the researchers hoped that at least 25% of the enrolled patient pool would have rare or uncommon cancers—ie, something other than colon, rectal, breast, non-small cell lung, or prostate tumours.
As the trial progressed, however, the actual number grew to about 60% of the participants. All told, NCI-MATCH enrolled 1,201 people in 39 different arms.
By matching patients to targeted therapies based on genetic mutations, NCI-MATCH showed that advanced cancer patients might benefit from using genomic sequencing in treatment planning.
Knowledge obtained from NCI-MATCH has opened the door for further precision medicine studies, including:
- ComboMATCH, which is similar to NCI-MATCH, will instead test combinations of drugs instead of single drugs.
- MyeloMATCH, which will test therapies based on genetic changes in the cancer cells of patients with acute myeloid leukaemia (AML) and myelodysplastic syndromes (MDS).
While NCI-MATCH is no longer enrolling new participants, the publication of some results has already begun. Patient follow-up is expected to continue for 3 years.
mRNA vaccine for pancreatic cancer
Following the notable success of mRNA vaccines for COVID-19, interest was greatly renewed in other applications of the technology.
Pancreatic cancer is one of the deadliest types of solid cancer, with a 5-year survival rate of less than 10%. By the time it’s detected, the cancer is usually advanced and has often metastasised. And in the limited cases where it's detected early enough for surgery to be performed, the recurrence is extremely high.
Personalised mRNA vaccines hold significant potential to treat pancreatic cancer more effectively. With a vaccine that targets unique cancer cell features in each patient, the immune system can be trained to find and attack these cells to a more significant effect.
This approach may provide a promising new treatment option for pancreatic cancer patients and could potentially be combined with current therapies to improve their overall effectiveness and patient outcomes.
Recent results from a phase 1 trial run by the Memorial Sloan Kettering Cancer Center demonstrated that a personalised mRNA vaccine could stimulate an immune response in patients with pancreatic ductal adenocarcinoma (PDAC). PDAC accounts for more than 90% of pancreatic cancer cases.
Disclaimer: This story is contributed by Tolu Ajiboye and is a part of our Global Content Initiative, where we feature selected stories from our Global network which we believe would be most useful and informative to our doctor members.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries