Hypernatraemia in Critical Care
M3 India Newsdesk May 02, 2024
The article provides insights into hypernatraemia, detailing its origins from water deficit relative to solute, and various aetiological factors including dehydration and renal dysfunction. It also emphasises careful management to avoid complications like cerebral oedema.
hypernatraemia is a disorder of water metabolism and is usually defined as a plasma sodium concentration above 145 mEq/L. hypernatraemia is characterised by a net loss of body water relative to sodium, which can occur with or without a decrease or gain in body sodium content. hypernatraemia is particularly common in critically ill patients.
Aetiology
1. The basic mechanisms of hypernatraemia are water deficit and excess solute. The most prevalent cause of hypernatraemia is excessive bodily water loss in comparison to solute loss.
2. hypernatraemia is typically accompanied by hypovolemia, which can develop under situations that result in combined water and solute loss, where water loss exceeds salt loss or free water loss.
3. Combined loss can be seen in extra-renal conditions such as gastroenteritis, vomiting, prolonged nasogastric drainage, burns, and excessive sweating. Exercise, fever, or prolonged exposure to intense temperatures can all cause excessive sweating.
4. Renal losses can be seen in intrinsic renal disease, post-obstructive diuresis, and with the use of osmotic or loop diuretics. Common causes of osmotic diuresis include hyperglycemia and mannitol.
5. Free water loss is seen with central or nephrogenic diabetes insipidus (DI) and also in conditions with increased insensible loss. Central DI can arise when ADH is not produced in sufficient quantities.
- Common causes of central DI are idiopathic, head trauma, cranial neoplasm, and pituitary infiltrative diseases, such as sarcoidosis and histiocytosis.
- Nephrogenic DI is caused by tubular insensitivity to ADH action and can be inherited in an X-linked pattern or acquired after taking certain drugs such as lithium, foscarnet, and demeclocycline.
6. Rarely, hypernatraemia with inadequate fluid intake can be seen in breastfed babies, child or elder abuse, and patients with an impaired thirst response.
7. Excess sodium is usually iatrogenic and seen in the hospital setting but can be associated with improper formula mixing, excess sodium bicarbonate ingestion, salt tablet poisoning, hyperaldosteronism, and seawater drowning.
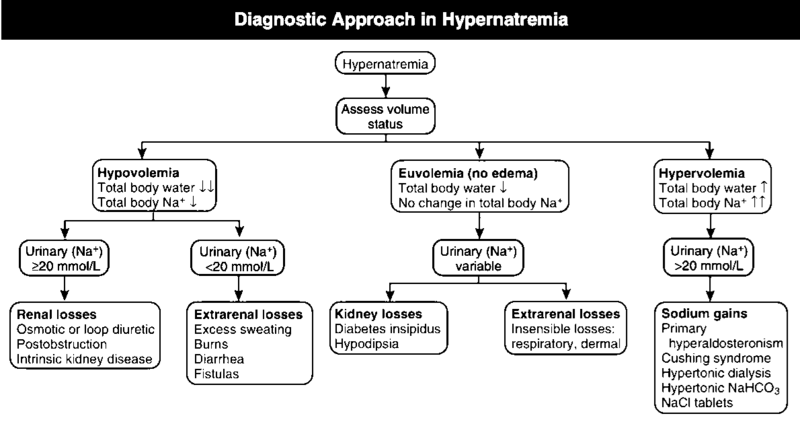
Approach
History and physical examination
- The majority of patients present with symptoms of fluid loss and clinical evidence of dehydration. Hypernatraemia symptoms and signs appear as a result of central nervous system dysfunction when serum sodium levels rise fast or exceed 160 mEq/L.
- Infants and Children present with irritability and agitation, which can progress to lethargy, somnolence, and coma.
- Patients with diabetes insipidus present with polyuria and polydipsia.
- Intracellular water loss can leave the skin feeling doughy or velvety. Orthostatic hypotension and tachycardia are usually present in hypovolemic hypernatraemia. The patient may experience heightened tone, rapid reflexes, and myoclonus.
Evaluation
- Plasma volume, osmolality, urine volume, concentrating ability, and osmolality can all aid in distinguishing between renal and extrarenal causes.
- In DI, urine is improperly diluted, with normal urine volume and urine osmolality smaller than serum osmolality.
- When DI is suspected, a water deprivation test may be conducted with desmopressin. In central DI, desmopressin administration demonstrates an increase in urine osmolality, while in the nephrogenic variety; there is no response to desmopressin.
- In extrarenal causes, the body attempts to preserve fluids by maintaining a low urine volume, a high specific gravity, and urine osmolality greater than serum osmolality.
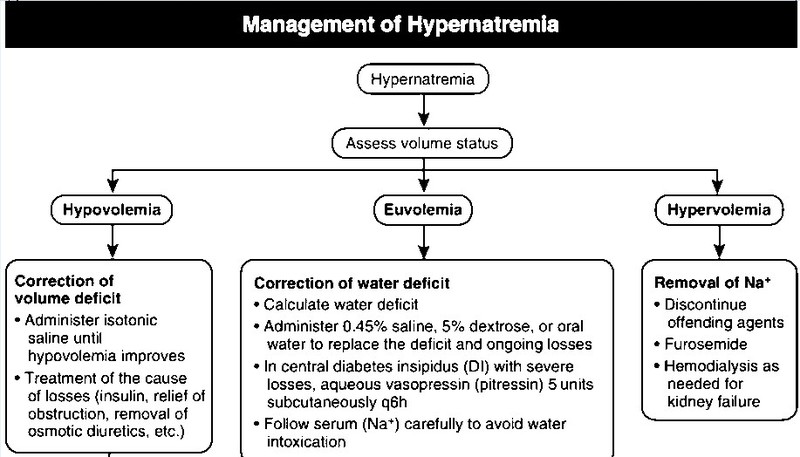
Treatment
- The proper treatment of hypernatraemia is recognising the underlying condition and addressing hypertonicity.
- The goal of therapy is to improve both serum sodium and intravascular volume. Fluids should be administered orally or via a feeding tube whenever possible.
- The first step in treating severe dehydration or shock in patients is fluid resuscitation with isotonic fluids, followed by free water correction.
- hypernatraemia is treated by calculating the free water deficit using one of the formulas below.
- Total Body Water[0.6 in men and 0.5 in women x body weight(kg)] x [(plasma sodium/140) -1]
- 4ml x bodyweight x (the required change in serum sodium mEq/L)
- It is important to remember that rapid correction of hypernatraemia can lead to cerebral oedema because water moves from the serum into the brain cells. The goal is to reduce serum sodium levels by no more than 12 mEq in 24 hours.
- Close serial monitoring of serum sodium every 2 to 4 hours is essential during the acute phase of correction.
- Seizures occurring during the correction of hypernatraemia are a sign of cerebral oedema due to rapid shifts in osmolality, and the administration of hypotonic fluids should be halted.
- The estimated free water deficit should be corrected over 48 to 72 hours with a decrease in serum sodium not exceeding 0.5 mEq per hour. Patients should be closely watched for their pace of correction, urine production, and continued losses.
- In cases of sodium intoxication, the free water need might be excessive, resulting in volume overload, necessitating the use of loop diuretics and, in certain cases, peritoneal dialysis to remove excess sodium.
- Desmopressin, which is available in both intranasal and oral forms, may be required for older children and adults suffering from central DI. Water intoxication and hyponatraemia are adverse effects seen with the use of desmopressin.
- Use of dDAVP(desmopressin): Oral tablet start with 100ug HS and up titrate to 200ug twice a day or nasal spray 10ug per spray 1-4 sprays divided over three doses.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Bhavin Mandowara is a practising nephrologist at Zydus Hospital, Ahmedabad.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries