Foetal Growth Restriction: Diagnosis of Late-onset
M3 India Newsdesk Aug 20, 2024
Throughout a pregnancy, Foetal Growth Restriction FGR can start at any time. Organ, tissue, and cell growth as well as the baby's total size may be impacted by FGR. This article explains the diagnosis of FGR and also discusses the importance of prenatal care.
Definitions
1. Foetal Growth Restriction FGR is defined as an estimated foetal weight (EFW) or abdominal circumference (AC) <10th percentile for gestational age due to pathologic factors[1]. There is variation among international society guidelines, with some including AC thresholds <10th or ≤5th percentile alone as a diagnostic criterion [2,3].
2. Severe FGR is defined as an EFW or AC <3rd percentile for gestational age. Severe FGR are at higher risk for perinatal morbidity and mortality at any gestational age at birth.
3. Early-onset FGR (without congenital anomalies) defines FGR as being identified before 32 weeks of gestation [4].
4. Late-onset FGR (in the absence of congenital anomalies) defines FGR identified at ≥32 weeks of gestation [4]. It is more common than early-onset FGR and it is associated with lower risks for perinatal morbidity and mortality, but neurodevelopment may be impaired [5].
5. Small for Gestational Age (SGA) is defined as a newborn birth weight <10th percentile for gestational age [1]. This definition does not make a distinction between newborns who are constitutionally small and not at risk for additional morbidity and those who are small because of growth restriction.
Diagnosis
Growth velocity
An abnormal growth velocity (a percentile drop between consecutive ultrasound scans of >50 percentiles in EFW or AC [eg, from the 75th percentile to the 20th percentile]) appears to predict perinatal complications (eg, preterm birth, preeclampsia, neonatal morbidity).
Abnormal Doppler velocimetry of the uterine arteries and foetal vessels (eg, umbilical, middle cerebral, ductus venosus) suggests reduced perfusion of the placental villous vasculature from both the maternal and foetal compartments.
Umbilical artery Doppler (fig.1,2)
UA Doppler becomes abnormal when embolisation damages 30 per cent of the placental villous vasculature [6]. When 60 to 70 per cent of the placental villous vasculature is obliterated, flow in the UA can become absent or even reversed at the end of the cardiac cycle.
The commonly used UA Doppler indices for clinical practice are:
- Pulsatility index (PI = peak systolic velocity - end-diastolic velocity/time-averaged maximum velocity)
- Resistance index (RI = peak systolic velocity – end-diastolic velocity/peak systolic velocity)
- S/D ratio: Peak systolic velocity/end-diastolic velocity
The UA Doppler abnormalities correlate well with prognosis and reversed diastolic flow is associated with fivefold higher perinatal mortality compared with absent flow.
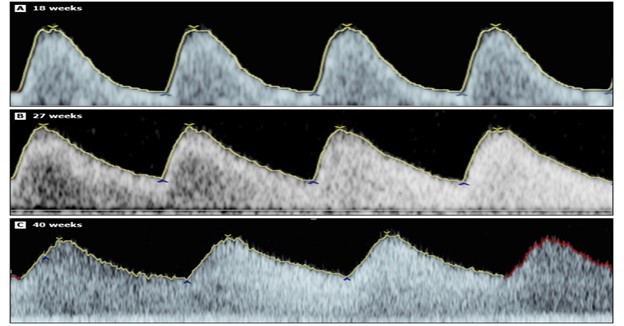
Fig. 1 Umbilical artery Doppler waveform in advancing gestational age in normal foetus. Note the diastolic flow increases with the gestational age.
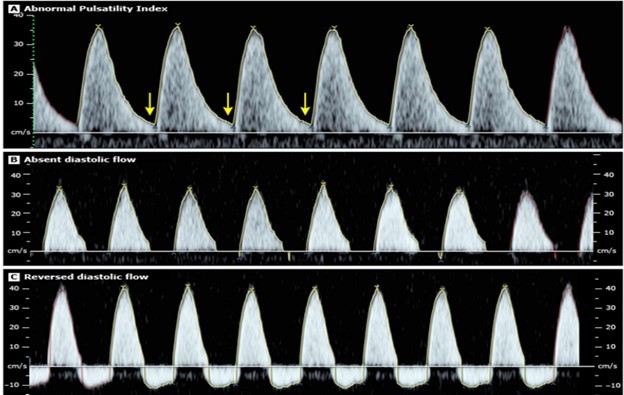
Fig.2 Umbilical artery Doppler flow velocity waveform in foetal growth restriction.
Middle cerebral artery pulsatility index (fig. 3): In uncomplicated pregnancies, vascular resistance of the foetal brain changes with advancing gestation, thus the middle cerebral artery (MCA) PI is low at early gestational ages (<20 weeks), then gradually increases, before gradually decreasing in the third trimester [7]. However, in foetuses such as those with FGR experiencing progressive hypoxemia, cerebral blood flow increases to compensate for the decrease in available oxygen (brain-sparing effect), which results in a reduction in MCA PI. Subsequent normalisation of the MCA PI may occur and is considered an ominous sign because it indicates the loss of brain-sparing.
The MCA PI can be the first parameter to become abnormal in late FGR, followed by the UA PI. An abnormal MCA PI is found in approximately 20 per cent of FGR cases with normal UA PI in the third trimester and is associated with a higher incidence of suboptimal neurodevelopmental outcome at two years of age compared with a normal MCA PI.
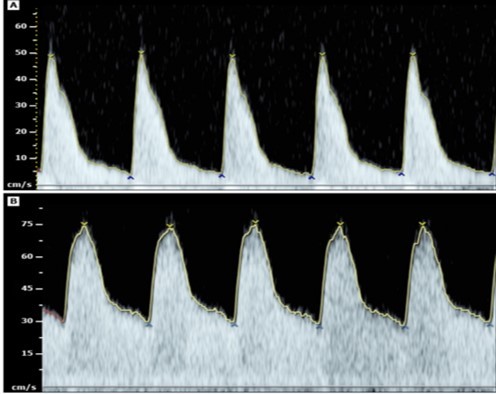
Fig.3: middle cerebral artery Doppler flow velocity waveform in A- normal growing foetus, B- foetal growth restriction. (note the high diastolic flow in B and also high peak systolic velocity)
Ductus venous Doppler (fig.4)
With the progression of the severity of FGR, and late in the course of the disorder, the a-wave becomes absent or reversible. Absent or reversed a-wave occurs more often in early than late FGR.
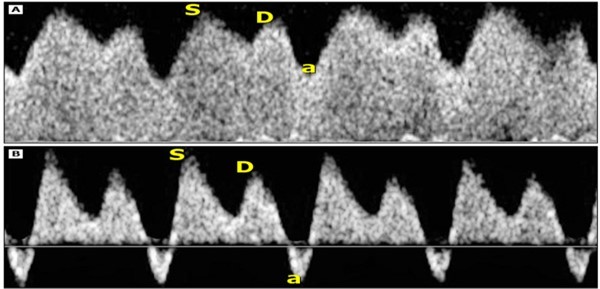
Fig.4: Ductus venosus doppler in normal growing foetus A and growth-restricted foetus B at 27 weeks of gestation. Note the reversal of a-wave.
Biophysical profile and nonstress test/cardiotocography: Both the nonstress test (NST; also called cardiotocography [CTG]) with amniotic fluid volume determination and the biophysical profile (BPP) are used to monitor foetal status as these tests evaluate both acute and chronic foetal physiologic parameters [8,9]The rationale for including a BPP in FGR management is based on its superior reflection of current foetal acid-base balance, which is independent of foetal heart rate testing and multivessel Doppler [10].
Cerebroplacental ratio: The cerebroplacental ratio (CPR) is the MCA PI divided by UA PI [11]. The CPR reflects both the placental status and foetal response and thus may be a sensitive Doppler index for predicting perinatal outcome [12]. In late-onset FGR, reduction in the CPR may be the only Doppler change present [13].
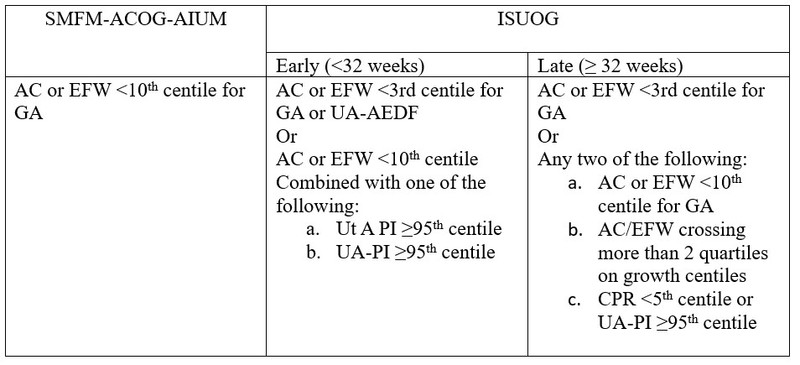
US and ISUOG diagnostic criteria for foetal growth restriction
Prenatal care
Goal
The focus of prenatal care in pregnancies with FGR is to identify those foetuses who are at the highest risk of perinatal demise and thus may benefit from early delivery.
If the UA and MCA Doppler (if performed because of late-onset FGR) are normal (UA pulsatility index [PI] ≤95th and MCA PI ≥5th percentile), then UA and MCA Doppler and a BPP are performed at weekly intervals.
If either the UA or MCA Doppler (if performed because of late-onset FGR) is abnormal but the UA has diastolic flow (UA PI >95th and MCA PI <5th percentile), amniotic fluid volume is normal, and no concerning maternal or foetal comorbidities exist, then UA and MCA Doppler are performed twice a week and a BPP is also performed at one of the visits and an NST is performed at the other visit.
If the UA Doppler has absent or reversed diastolic flow, then the patient is admitted for convenient access to frequent foetal surveillance and to enable prompt foetal evaluation in the event of decreased foetal activity or other pregnancy complications. NSTs are performed every 6 to 12 hours, a BPP is performed daily, and UA and MCA Doppler are performed two to three times per week.
These foetuses are also monitored with DV Doppler. Absent or reversed DV a-wave in this setting represents an advanced stage of foetal compromise and can be an additional factor to consider during counselling and shared decision-making; however, this finding alone is not an indication of delivery.
Maternal interventions
There is no convincing evidence that any intervention in an otherwise healthy pregnant patient improves foetal growth and outcome in FGR.
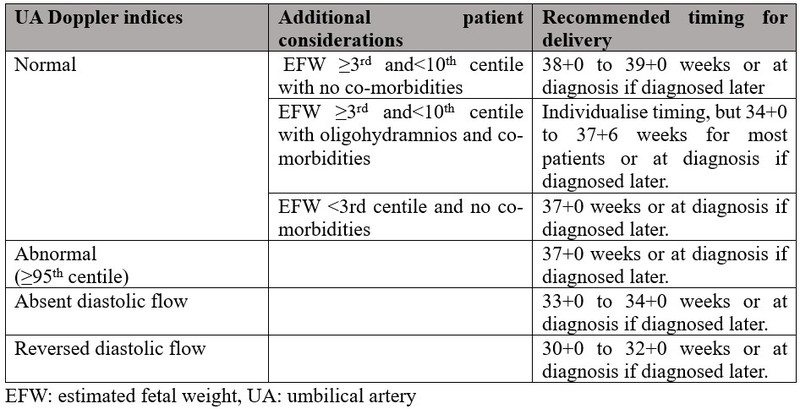
Table 2: Delivery timing in case of foetal growth restriction based on UA Doppler and weight
Route
Cesarean birth is performed for standard obstetric indications; otherwise, a trial of labour is acceptable. Intrapartum foetal monitoring – Continuous foetal heart rate monitoring is indicated, given the increased potential for foetal hypoxemia during labour.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Supriya Chaubey is an Assistant professor at HIMSR, New Delhi.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries