Emergency Management of Hyperglycemia
M3 India Newsdesk Oct 04, 2023
The article emphasises hyperglycemia, DKA, and HHS while putting a focus on early detection, treatment, ongoing patient education, and lifestyle control for better diabetes outcomes.
Hyperglycemia is commonly diagnosed when the blood glucose is greater than 125 mg/dL while fasting, and greater than 180 mg/dL two hours postprandial. Common etiologies include reduced insulin secretion, decreased glucose utilisation, and increased glucose production.
Presentation
In patients not known to have diabetes
Symptoms and signs like polyuria, polydipsia, polyphagia and/or weight loss, particularly in children and young adults, should prompt urgent point-of-care capillary blood glucose checking.
In patients with a known diagnosis of diabetes
Symptoms and signs in the patient with an acute illness and/or persistent hyperglycemia should be considered a potential hyperglycemic emergency.
There are 2 main hyperglycemic emergencies
1. Diabetic Ketoacidosis - DKA is an acute, life-threatening emergency characterised by hyperglycemia and acidosis.
2. Hyperosmolar hyperglycaemic states - HHS refers to severe persistent hyperglycemia, in the absence of ketosis, but accompanied by profound dehydration.
Some factors associated with an increased risk of hyperglycemic emergencies
Children and young people with known type 1 diabetes:
- Unstable glycemic control
- Medication non-compliance - especially insulin
- Previous DKA
- Acute infection and sepsis
- Pancreatitis
- Trauma, surgery or burns
- Medications - corticosteroids, atypical antipsychotics, immunosuppressive agents, SGLT2i
- Alcohol and recreational drug use
- In the elderly - signs of DKA may be subtle, but mortality rates may be higher
- Pregnancy
Evaluation and initial investigations
When evaluating a patient for hyperglycemia, the focus should be on the patient's cardiorespiratory status, mental status, and volume status. The following investigations are usually done:
- Bedside capillary blood glucose
- Venous plasma glucose
- Blood gas for determining acidosis
- Serum and urine ketones
- Complete blood count and electrolytes
- HbA1c
Treatment guidelines
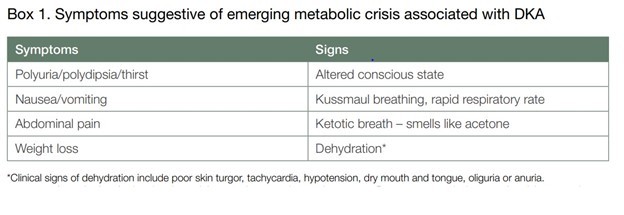
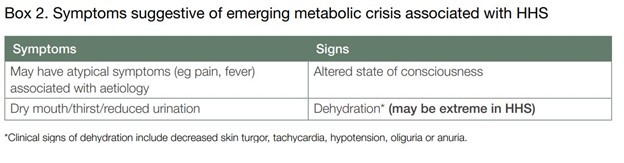
These images provide an overview of how to treat DKA and HHS.
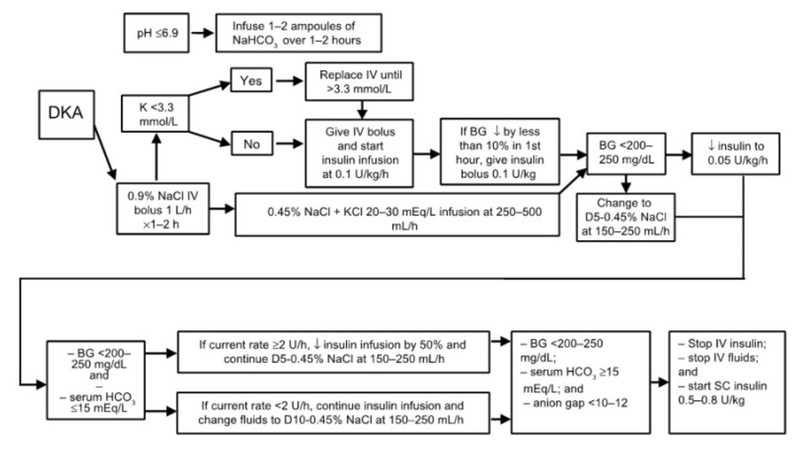
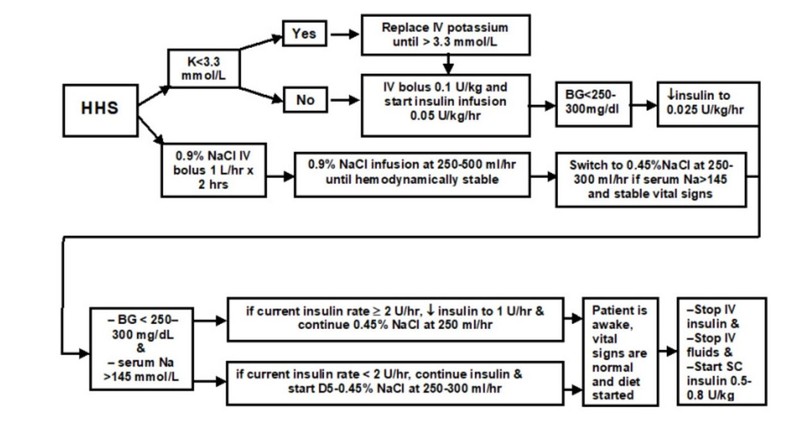
Fluid resuscitation
The IV fluid of choice in the management of DKA or HHS is Isotonic saline (0.9% Saline). Saline should be started at a rate of 10-20 ml/kg. At least 1 L of fluid should be administered within the first hour of the presentation. Over the next 8 hours, 0.9% sodium chloride should be given in combination with potassium chloride to correct overall K+ depletion.
- 1 L over 2 hours
- 1 L over 2 hours
- 1 L over 4 hours
The patient should be re-evaluated regularly to assess the need for further fluid resuscitation or a change in the rate of infusion.
Insulin Therapy
Insulin is administered by Fixed Rate IV Insulin Infusion (FRIII). The infusion dose is set based on the weight of the patient in kg. The dose is set at 0.1 units/kg/hour.
Prior to FRIII, a bolus dose + Variable Rate IV Insulin Infusion (aka VRIII/Sliding Scale) was the norm. However, there were some shortcomings to this. VRIII is disadvantageous, as it is based on capillary blood sugar. Using a sliding scale allows for control of blood sugars but does not facilitate the reduction of ketogenesis adequately.
Potassium correction
Although serum potassium may be normal or high at initial presentation, there is an overall depletion of total body potassium in DKA. Potassium depletion occurs due to a shift in potassium from intra to extracellular space through the H-K pump. The K+ is then lost through osmotic diuresis.
Treatment goals
0-60 minutes (T=0 when first IV fluid is started)
- Commence IV fluid resuscitation with 0.9% saline
- Begin Insulin infusion using FRIII
- Hourly monitoring of blood glucose and serum ketones
- 2 hourly K+ and HCO3 monitoring (up to 6 hours)
- Re-evaluate the patient clinically and closely monitor vitals
At this point, one should assess ABC, obtain IV access, assess GCS look for drop-in sensorium, and follow up on the lab reports.
60 minutes to 6 hours
- Fall of serum ketones by 0.5 mmol/L/hr OR
- Rise of bicarb by 3 mmol/L
- Fall of glucose by 50 mg/dL/hr
- Maintain serum potassium
- Prevent the patient from entering the hypoglycemic state
- Continue monitoring hourly BG, ketones and 2 hourly monitoring of K+ and HCO3
If there is no change in blood glucose or ketones, increase insulin infusion by 1 unit/hour until targets are achieved. Consider catheterisation if anuric/incontinent. Maintain a fluid intake/output chart.
6 to 12 hours
- Continue IV fluid replacement and insulin infusion
- Monitor electrolyte and acid-base imbalance
- Evaluate the patient, ensuring clinical improvement
- Monitor complications that may arise secondary to treatment (cerebral oedema, fluid overload)
- Prevent hypoglycemia
- Treat precipitating factors
Reassess cardiac status. Alter infusion rate of IV fluid if required. At 6 hours, check for resolution of DKA: serum ketones <0.3 mmol/L, Venous pH of greater than 7.3 (bicarb should not be used as a parameter at this stage).
12 to 24 hours
- Ketonemia and acidosis are expected to be resolved in 24 hours.
- Ensure that metabolic and electrolyte abnormalities continue to improve or have returned to normal.
- Attempt oral fluids/feeds. If tolerated, continue SC insulin administration.
- If the patient does not take oral feeds, IV fluids should be resumed and insulin should continue using VRIII.
- Check for resolution. If unresolved, continue FRIII and fluid resuscitation.
Resolution
- Ketonemia < 0.3mmol/L
- pH > 7.3
- Resolution is usually expected around 24 hours after the commencement of treatment
- By this time, we expect the patient to be eating and drinking normally and SC insulin to be restarted
Restarting regular insulin
- Regular SC insulin can be restarted once serum ketones < 0.3 and pH >7.3.
- IV insulin is to be discontinued 30 minutes after SC insulin administration.
- Long-acting insulin is preferred when restarting a normal regimen as it reduces the occurrence of rebound hyperglycemia.
Preventive care and patient education
Every patient is different, and their presentation may be atypical, but from the clinician’s standpoint the following preventive approaches can help prevent a readmission or developing complications of hyperglycemia:
- Teach the patient how to consistently self-monitor blood glucose levels, and to maintain a journal if possible.
- Educate the patient on the need for tightly controlled glucose levels of 80 to 120 mg/dl before meals and less than 180 mg/dl 2 hours after eating.
- Teach the patient about the importance of annual eye, foot, and kidney function screenings to monitor vascular complications. We can refer to an ophthalmologist for yearly eye exams.
- Monitor HbA1c levels every 6 months.
- Educate about the importance of maintaining the blood pressure to less than 130/80 mmHg.
- Initiate statin therapy if the patient has hyperlipidemia.
- Collaborate with a nutritionist to educate the patient about adopting a low glycemic index diet.
- Educate the patient about weight reduction if the patient is overweight or obese. Provide an individualised weight loss goal.
- Instruct the patient about the importance of increasing physical activity to reduce glucose levels.
- Teach the patient the signs and symptoms of hyperglycemia (e.g., frequent urination, altered mental status, nausea and vomiting, and increased thirst) and provide instructions on when to seek additional care.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr. Christus Gerald Herbert, Fellowship in Diabetology, AFIH, Lead Assistant Manager, SCIO Health Analytics, Chennai.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries