Early Childhood Caries: Developmental Stages & Management
M3 India Newsdesk Aug 16, 2024
Oral health is an integral part of general health. Maintaining good oral health includes more than having healthy teeth, due to the presence of active and uncontrolled caries. This article explains the prevalence, pathogenesis and prevention of Early Childhood Caries ECC.
Microbial disease of calcified structures of the teeth characterised by demineralisation of inorganic constituents and destruction of organic content.
-WHO
Previous terminologies:
- Baby bottle tooth decay
- Nursing bottle syndrome
- Nursing caries (Arkin,1986; Ripa 1988)
Definition of early childhood caries ECC
AAPD 2016 - ECC is defined as one or more decayed (non-cavitated or cavitated lesions), missing (due to caries) or filled tooth surfaces in any primary tooth in a child 71 months of age or younger.
The definition of severe early childhood caries (S-ECC) is any sign of smooth-surface caries in a child younger than three years of age, and from ages three through five, one or more cavitated, missing (due to caries), or filled smooth surfaces in primary maxillary anterior teeth or a decayed, missing, or filled score of greater than or equal to four (age 3), greater than or equal to five (age 4), or greater than or equal to six (age 5).
Global prevalence of ECC
- ECC is a public health emergency
- It is 12th on the list of 291 most common childhood diseases [Vos et al, 2012]
- Global Prevalence of ECC = 48% (Uribe SE et al Int J Ped Dent, 2021)
Prevalence of ECC in India
- The overall prevalence of ECC in India - 49.6%
- Andhra Pradesh - highest prevalence of ECC - 63%, and the lowest prevalence was reported in Sikkim (41.92%)
- The government should identify ECC as a national priority which requires significant attention
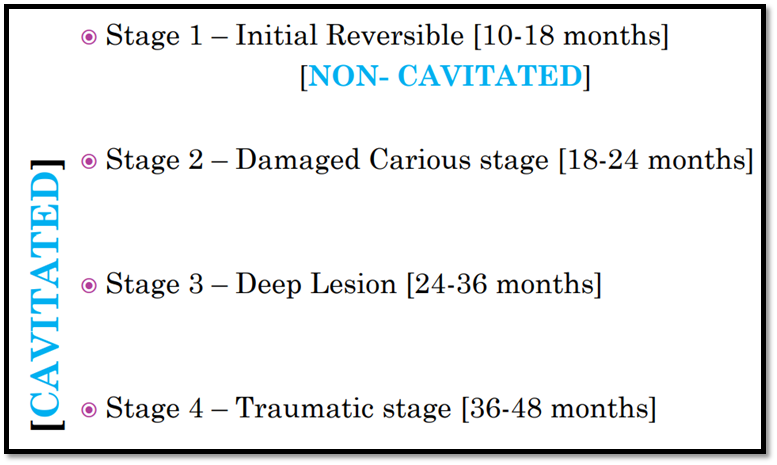
Developmental stages of ECC
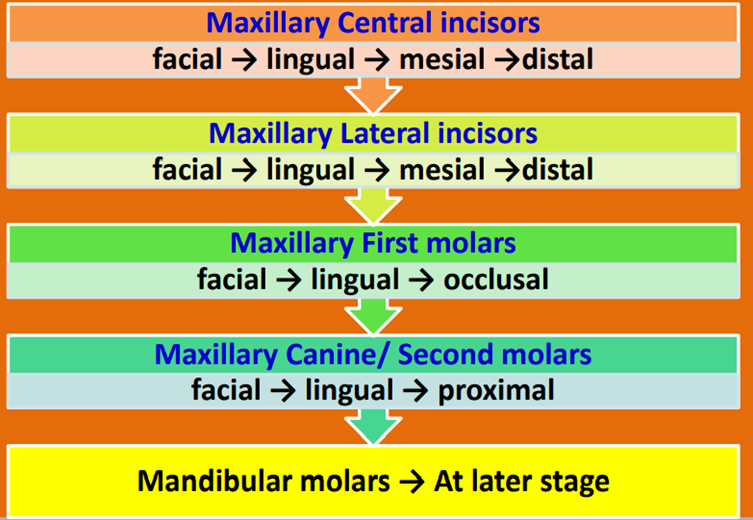
According to Veerkamp & Weerheijm(1995), the developmental stages of ECC are as follows:
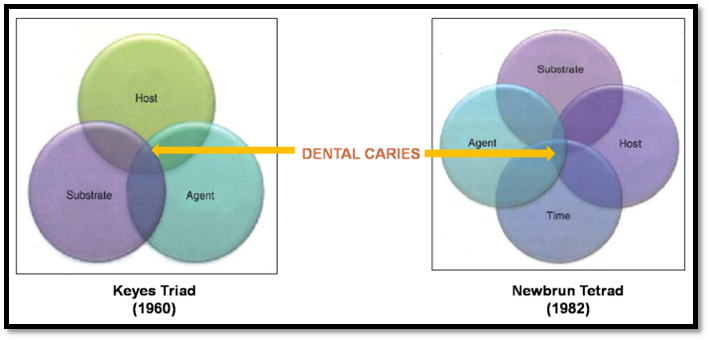
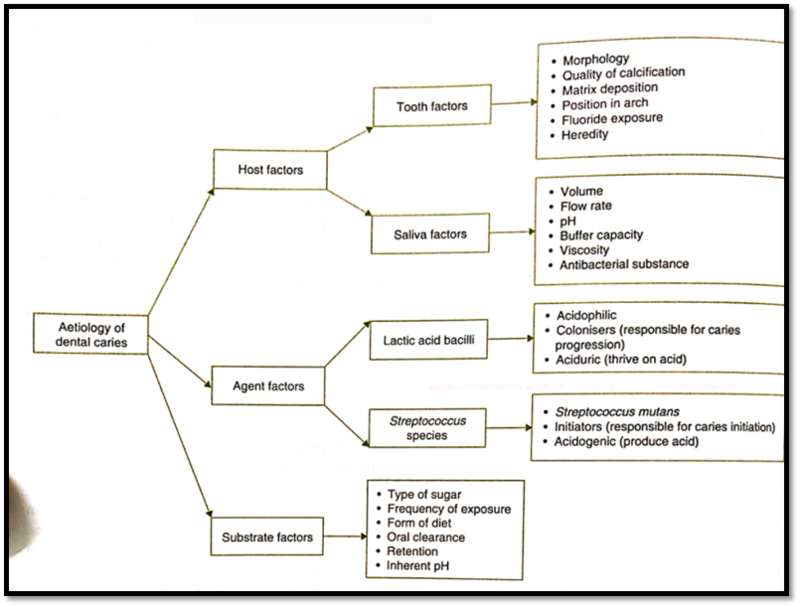
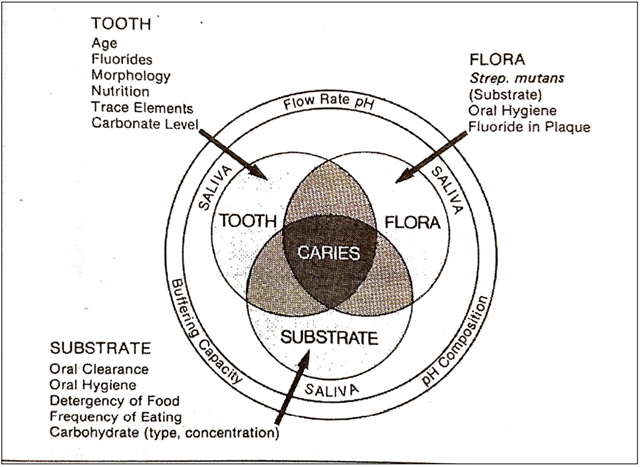
Aetiology/ Causal factors
Pattern of caries progression
Pathogenesis of ECC
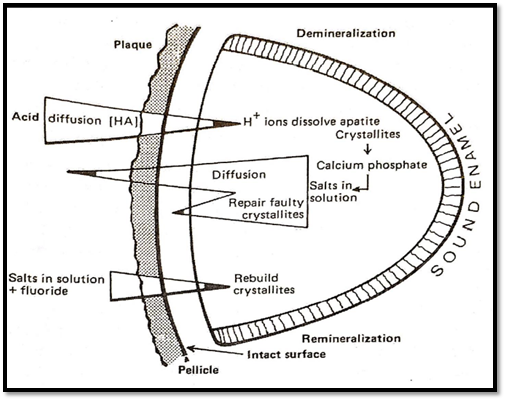
Demineralisation- Remineralisation at the crystal level
1. At pH below 5.5 – Demineralisation occurs,
Ca10(PO4 )6 (OH)2 + 10 H --------> 10 Ca2 + 6H(PO4)3- + 2H2O
[Lactic acid] [ hypophosphate ion]
Voids are formed in enamel and the surrounding saliva becomes supersaturated with Ca2+ and unstable phosphate ions.
2) When pH rises back to neutral pH and the buffering action of saliva,
H2O + CO2 H2CO3 [ Carbonic acid – WEAK ACID] formed
3) To re-establish the equilibrium pressure of CO2, the decomposition of H2CO3 occurs
H2CO3 HCO3 --------> (CO3) 2- + Bubbling of CO2
[Bicarbonate ion] [Carbonate ion]
4) Remineralisation occurs
Consequences of ECC
The reason behind ECC becoming a public health problem is as follows:
- High risk for new carious lesions (primary/ permanent)
- High treatment costs
- Medical Expenditure Panel Survey 2015
- Hospitalisations & emergency room visits
- Loss of school days
- Diminished ability to learn
- Diminished Oral health-related Quality of life
Quality of life and early childhood caries
- Spreads faster to multiple teeth
- Early involvement of the pulp
- Usually affects teeth surfaces which are immune to decay
- Difficulty in eating hard chewable food substances
- Difficulty to brush
- Sensitivity to thermal changes and physical stimuli
- Frequent episodes of cough, cold etc
- Poor general health because of poor intake of solids
- Difficulty to sleep (Constant pain or sensitivity on teeth)
Prevention
1. Primary prevention
Primary prevention for ECC needs to begin before the initiation of the disease and is the key to reducing the worldwide prevalence of ECC. It involves educational information and preventive therapies - accessible to the parents/caregivers.
Strategies used:
A. Tooth brushing: Brushing with Fluoridated toothpaste
Brushing helps in two ways;
- Disrupting the biofilm.
- Recharging the plaque by any anticancer agent e.g. fluoride.
Three important factors in brushing:
- Frequency
- There is strong evidence that infrequent brushing leads to a greater incidence of dental caries
- It is recommended to brush at least twice daily
- Duration
- It is recommended to brush for at least two minutes.
- Type of dentifrice
- Use fluoride toothpaste- helps in both the prevention of caries and remineralisation of early WSLS
- Minimum concentration 1000 ppm
- WHO recommends - affordable fluoride toothpaste for everyone
- Brushing to prevent ECC
- Tooth wipes - Effective & acceptable method in removing biofilm from babies' teeth
- Amount of toothpaste
- Children should spit out, not swallow and not rinse
- < 2 years: smear
- 2-6 "Pea-sized"
- 6-12 years: 3/4 length
- >12 years: full length
- Rinsing with a wet brush; helps to retain fluoride
Optimal exposure to dietary fluoride is important and can be delivered by fluoridated water, fluoridated salt, and fluoridated milk.
B. Diet modification
- Avoiding night-time bottle feeding with milk or drinks containing free sugars.
- Avoiding baby bottles and breastfeeding beyond 12 months.
2. Secondary prevention
- It aims to prevent the progression of, or stimulating the regression (remineralisation) of, caries, before the cavitation stage of lesions.
- It includes:
- More fluoride applications
- Pit and fissure sealants
- Resin infiltration for non-cavitated lesions
- Remineralising agents
3. Tertiary prevention
It can involve both non-invasive and invasive preventive management. Tertiary prevention aims to control diseases and functional rehabilitation.
These include:
- SDF
- Conservative caries removal ART
- Glass ionomer restorations
- Resin Composite restoration
- Pulp procedures
- Full coverage crowns
Recent advances in caries management
- Antimicrobial peptides
- Probiotics
- Prebiotics
- Sugar polyols
- Natural products
- Quorum-sensing targets
- Fluoridated hydroxyapatite-coated preformed metal crowns
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Neha Kalantri is a practising dentist from Nashik.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries