Dr. Vanita Raut explains the newest long-acting reversible contraceptive (LARC)
M3 India Newsdesk Jul 29, 2019
Dr. Vanita Raut writes about and explains the use of the newest long-acting reversible contraceptive (LARC) which requires a convenient, sub-dermal insertion- the radiopaque, progesterone only Etonorgestrel Implant.
Family planning is a cost-effective way to save the lives of women and children and empower families to determine the optimal timing and spacing of births. Contraceptives, therefore, have to be highly effective, user-friendly, with minimal side effects; they require counselling before treatment.
At present, there are many long-acting reversible contraceptives (LARC) available. Etonorgestrel Implant (IMPLANON NXT, MSD, Organon) is a newer sub-dermal LARC.
It is a radiopaque, non-biodegradable, progesterone only, flexible implant. It comes as soft, flexible rod preloaded in a sterile ready for use disposable applicator. It is 4 cm in length and 2 mm in diameter.
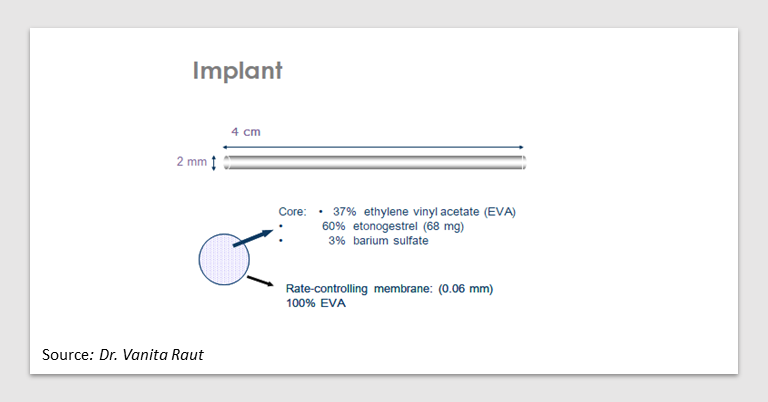
Each implant contains 68 mg of Etonorgestrel which gets released everyday over a period of 3 years. The release rate is approximately 60-70 mcg/day in week 5-6 and decreases to approximately 30-40 mcg/ day at the end of second year and to approximately 25-30 mcg/day at the end of the third year.
Mechanism of action
The main contraceptive action is by inhibition of ovulation. It also thickens cervical mucus making it impenetrable for sperms and thins the endometrium thus preventing implantation of fertilized egg.
Indications: For contraceptive purpose
WHO eligibility criteria
- Extremes of reproductive age (Category 1)
- Breast feeding, post-partum, post abortion and post ectopic (Category 1)
- Obese, hypertensive, smokers(Category 1)
- Endocrine disorders(Category 1)
- PID, fibroids, anatomic abnormalities(Category 1)
- Neurological conditions (Category 1, 2)
- Cardiovascular disease (Category 1, 2)
Contraindications
- Steroid-dependent tumors
- benign or malignant liver tumors
- known or suspected breast cancer
- Known or suspected sex-steroid sensitive malignancies
- Active venous thromboembolic disorders
- Presence or history of severe hepatic disease when liver function values have not returned to normal
- Confirmed or suspected pregnancy
- Undiagnosed vaginal bleeding
- Hypersensitivity to the active substance or to any of the excipients of Implanon
Drug interactions
Efficacy of Implanon may be affected by concomitant use of enzyme inducing drugs:
- Anticonvulsants
- carbamazepine
- hydantoins (phenytoins)
- barbiturates
- oxcarbazepine
- Antituberculous, antifungal and antiviral medications
- Rifampicin
- Rifabutin
- Griseofulvin
- ARVs for HIV
- Other liver enzyme inducers
- St. John’s wort (hypericum)
Counselling of patient
- Counselling is very important for acceptance and more so for continuation of any contraceptive method. Advantages and limitations of hormonal implants should be explained.
- The woman should be told about the correct time of insertion and explain insertion and removal procedures.
- She should be informed about the common side effects especially about the changes in bleeding pattern.
- She should be given appropriate education material. Sufficient time should be provided for patient to review, consider and ask questions.
Timing of insertion
- Within first 5 days of menstrual cycle
- Within 5 days following first trimester abortion
- Within 21-28 days of 2nd trimester abortion
- Post-partum
- If breast feeding- after 4 weeks of delivery
- If not breastfeeding- between 21 to 28 days
Insertion
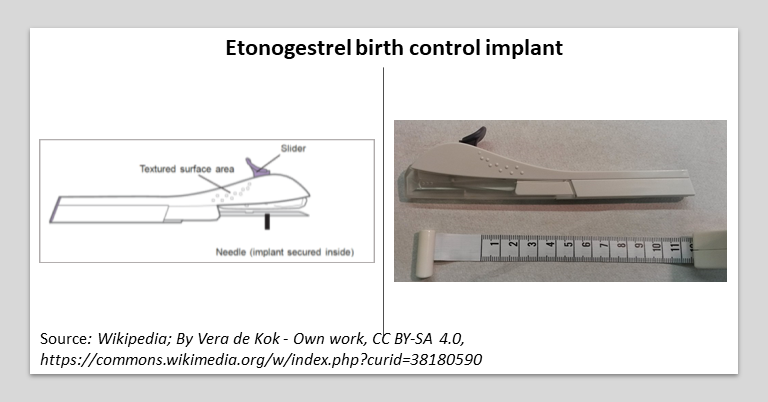
The healthcare professional has to be trained in the technique of insertion and removal of implant. It is inserted sub-dermally in the non-dominant arm under local anesthesia. The implant should be inserted just under the skin at the inner side of upper arm avoiding the sulcus between the biceps and triceps muscles and the large blood vessels that lie in the neuro muscular bundle deeper in the subcutaneous tissue. Immediately after insertion the presence of implant should be verified by palpation.
Removal of implant
- Timing:
- After active life (3 years) of implant is over
- Patient’s request
- Severe side effects
- It is removed by a very small incision under local anesthesia
Undesirable side effects/complications
- Insertion related side effects
- Migration, bent or broken implant
- Breast pain/ breast tenderness
- Menstrual irregularities
- Weight gain
- Headache, migraine
- Emotional lability, depression
Advantages of Etonorgestrel Implant
- Highly effective (99%)
- One time insertion
- Long acting progestogen sub dermal implant
- Immediate contraceptive efficacy
- Low incidence of side effects
- Benefits regarding dysmenorrhea
- Low impact on metabolic parameters
- Immediate return of fertility after removal
Disadvantages of Etonorgestrel Implant
- Requires minor surgical procedure for insertion and removal
- Training to healthcare provider is required for insertion and removal
The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
Dr. Vanita Raut is a Consultant Gynaecologist at a prominent Mumbai hospital. She has also served as the past President of Mumbai Obstetrics and Gynecology Society and as a former professor, Seth G S Medical College and KEM hospital, Mumbai.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries