"Doctor, can simple daily steam inhalation prevent COVID infection?": Prof. Dr. Sundeep Mishra answers
M3 India Newsdesk Jul 24, 2020
Prof. Dr. Sundeep Mishra clarifies frequently asked patient questions on whether steam inhalation and saline gargles help in COVID-19 and if so, which stages of the disease would they prove particularly useful. He also takes us through COVID-19 pathogenesis and timeline from exposure to symptom onset.
For our comprehensive coverage and latest updates on COVID-19 click here.
Prevention of COVID-19
After any viral infection the outcome is dependent on three factors:
- The properties of the infecting virus (in this case SARS-CoV-2)
- The circumstance of viral infection (dose and route of infection)
- Several host factors which include- age of the host, genetic susceptibility, ability to induct anti-inflammatory cells and proteins, presence of concomitant infections and past exposure to the same virus or cross-reactive agents
In the last issue (Part 1) we discussed how impacting the properties of SARS CoV (SARS coronavirus) we could affect the outcome. In this part, we will discuss how altering the virus load we could prevent COVID-19.
How to reduce viral load: Understanding and altering the modes of transmission & pathogenesis of SARS CoV
Various modes of transmission of COVID-19 virus
- Airborne transmission by infected people through respiratory droplets and contact routes
- Respiratory tract- Droplet transmission via respiratory tract when a person is in close contact (within 1 m) with someone who has respiratory symptoms (e.g. coughing/sneezing)
- Mucosa- Droplet transmission via mucosae (mouth or nose) or conjunctiva exposed to potentially infective respiratory droplets
- Transmission may also occur through fomites in the immediate environment around the infected person
- Direct contact with infected people
- Indirect contact with surfaces in the immediate environment or with objects used on the infected person (e.g. stethoscope, thermometer)
- Latrogenic airborne transmission
- Airborne transmission in specific circumstances in which procedures or support treatments that generate aerosols are performed e.g. endotracheal incubation, open suctioning, manual ventilation before intubation, non-invasive positive pressure ventilation, tracheostomy, and cardiopulmonary resuscitation.
Pathogenesis of COVID disease
Once an individual comes in contact with infectious material (respiratory droplet or fomite, COVID-19 can be divided into three phases that correspond to different clinical stages of the disease.
Stage 1: Asymptomatic state (initial 1–5 days of infection)
The inhaled COVID virus binds to epithelial cells in the nasal cavity and starts replicating. For a few days there is a logarithmic expansion of viral load and local propagation of the virus which evokes a limited innate immune response (no adaptive immunity).
Stage 2: Upper respiratory tract and conducting airway response (day 3-12) – Disease Stage
During the next few days the virus multiplies, propagates and migrates down the respiratory tract along the conducting airways, and now a more robust innate immune response is triggered; In ~80% of the infected patients, the disease will be mild and mostly restricted to the upper and conducting airways.
Stage 3: Hypoxia, ground glass infiltrates, and progression to ARDS – Serious Disease Stage
Unfortunately, ~20% of the cases may progress to stage 3 disease and will develop pulmonary infiltrates; some may develop very severe disease with fatality 2-5%.
COVID infection and elderly
Elderly individuals are particularly at risk because of their diminished immune response and reduced ability to repair the damaged epithelium. The elderly also have reduced muco-ciliary clearance, permitting easy access of virus to alveoli.
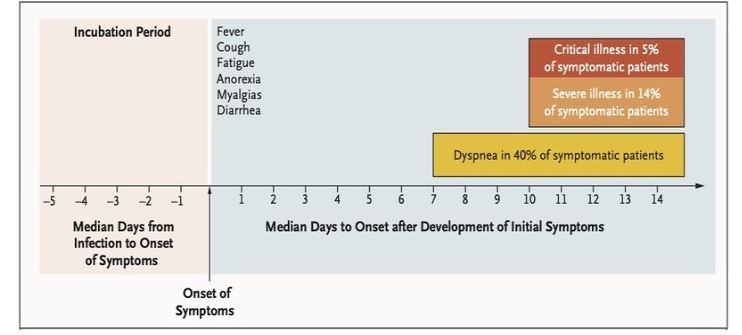
COVID timelines
It takes about 5 days from exposure to onset of disease (fever, cough, myalgia, etc) which persists for about 7 days when serious symptoms like dyspnoea start emerging. At this point, the chain of viral transmission may be prevented and viral load decreased by working on these modes of transmission.
Timeline of COVID-19
To limit virus load, the following strategies may be undertaken:
Social Distancing
Social distancing is a non-pharmaceutical infection prevention and control intervention implemented to avoid/decrease contact between those who are infected with a disease-causing pathogen and those who are not, so as to stop or slow down the rate and extent of disease transmission in a community. This eventually leads to a decrease in spread, morbidity, and mortality due to the disease. At an individual level, it involves
- Staying at home as much as possible; avoiding crowded places; restaurants, malls etc.
- Maintaining hygiene and physical distancing of ideally 2 meter (6 feet) at public places
- Doing away with shaking hands and hugging as a manner of greeting
- Avoiding contact with sick people
- Staying up to date on the latest COVID-19 hotspots (cities or local areas where COVID-19 is spreading widely)
- Avoiding traveling to places
General hygiene measures
General measures of hygiene for prevention of viral respiratory infections include following:
Hand hygiene: Hand washing with soap and water for at least 40-60 seconds. An alcohol-based hand sanitiser may be used and hands rubbed for 20-30 seconds, if soap and water are unavailable. Individuals should avoid touching their eyes, nose, and mouth with unwashed hands.
Respiratory hygiene: Coughs and sneezes should be covered with a tissue, followed by disposal of the tissue in the trash. In the absence of tissue/handkerchief, the patient should be instructed to cover their nose and mouth with their arms, with elbows flexed during coughing/sneezing. Spitting should be avoided.
Environmental hygiene:
- Individuals should avoid close contact with sick people
- Sick people should stay at home (eg, from work, school)
- Frequently touched objects and surfaces should be cleaned and disinfected regularly
- Disinfectants should be used on objects like phones, computers, and doorknobs
- Soap and water should be used for objects that are used for cooking or eating- like utensils and dishware
Face Masks
Face masks are an effective way of respiratory tract infection transmission.
Surgical facemask/cloth masks
Surgical face masks may be useful in preventing infection by rhinovirus, influenza virus, seasonal coronavirus [non-SARS-CoV-2 specifically] but a South Korean study revealed that it was ineffective in reducing the spread of COVID-19 virus from a symptomatic patient but because of their ability to block the respiratory droplets they may slow the transmission of SARS-CoV-2 virus in asymptomatic carriers. Thus, they may be useful when used in closed public places where temperature screening has already been undertaken.
N95 Filtering Face-piece Respirators (FFRs)
An N95 respirator is a facemask which blocks at least 95% of very small airborne particles down to 0.3 microns. They are assigned a protection factor (APF) of 10. APF of 10 means the N95 reduces the aerosol concentration to 1/10 of that in the room and this equates to blocking 90% of airborne particles from being inhaled (droplet particles through which COVID virus spreads). Because of its higher ability to block respiratory droplets they may be even more useful when worn in closed public places.
Powered Air Purifying Respirator (PAPR)
These are battery-powered respirators which are very effective in preventing spread of COVID infection in environs of symptomatically manifest patients. However, they are less user-friendly, restrict peripheral vision and are useful only for health-care professionals taking care of known COVID patients.
Face masks should not be worn:
- By children <2 years old
- By people who have breathing difficulty
- By people who are unable to remove their own masks
- While performing strenuous exercise
Wearing gloves
When visiting public places like local grocery shops or pharmacy, wearing gloves may seem a sensible precaution. They prevent fomite transmission from any contaminated surface to naked hands. However, gloves give a false sense of security especially if individuals touch other parts of the body with a contaminated glove like face and mouth. Moreover, the most tricky part of the process involves removing the gloves, wherein if not cautious, the germs may get transferred to hands and other parts of the body. Thus, hand hygiene is more important than wearing gloves.
Steam inhalation
SARS COV-2 is a crown-shaped virus; single-strand RNA with a lipid coat. Having a lipid coat, it is heat sensitive and rapidly loses viability/infectivity at 56°C in 15 minutes (10000 units per 15 minutes) and then rapidly losing thereafter (>3 log10) becoming completely non-viable at 70°C.
Likewise, higher relative humidity ( >95% at 38°C) also makes it un-infective. It is also inactivated by ultraviolet light, alkaline (pH >12), or acidic (pH <3) conditions. Thus, steam inhalation seems a logical solution to COVID infection. As per timelines (check the figure above), coronavirus remains and proliferates in the nasophrynx and upper respiratory tract for up to two weeks after exposure and is thus amenable to application of steam.
Therefore, steam inhalation may be especially useful in stage1 and stage 2 of the disease; high concentration of virus in the oropharynx in asymptomatic stage and high viral loads in the upper respiratory tract during early disease states. It might be of only a limited value in advanced disease infecting the lower respiratory tract.
Heated, humidified air has long been used by people with the common cold. GPs in Europe (Netherlands & UK) and the US often recommend it, and it is even included as a recommendation in guidelines and patient brochures issued by European & US medical practitioner societies.
The theoretical basis for this recommendation is that steam may help decongested inflamed mucus membrane of the upper respiratory tract better and may even destroy the cold virus as it does in vitro. Earlier, some trials have reported benefits of heated, humidified air for symptom relief in people with the common cold and only minor adverse events (including discomfort or nasal irritation).
On the other hand, enveloped viruses have very, very definite heat sensitivity, and thus coronavirus which is a lipid-enveloped virus is likely to be more heat-sensitive than other viruses. Thus, on the balance of logic and evidence and in view of very low side-effects of steam inhalation if done properly, there seems ‘no harm’ in employing this relatively cheap and user-friendly therapy. It is generally recommended for application twice a day (so that the viral colony is unable to develop).
Warm saline gargles
Saline gargles are a way of nasopharyngeal wash to prevent the virus from inhabiting and replicating in the nasal and pharyngeal mucosa. It may act by viral shedding thus reducing viral transmission in cases of viral acute respiratory tract infections. Frequent saline gargles with hypertonic saline (three teaspoons in ½ litre of water may help in maintaining naso-pharyngeal hygiene).
Conclusion
While social isolation, maintaining hand, respiratory, and environmental hygiene and wearing face masks are of definite help some other strategies like steam Inhalation and warm saline gargles may also help since there does not appear to be any significant downside (if done properly).
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
The author, Dr. Sundeep Mishra is a Professor of Cardiology.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries