Differential diagnoses of Dermatophytosis- Can Tinea mimick an STD or erythroderma?: Prof. Dr. D.G. Saple
M3 India Newsdesk Feb 03, 2021
In this part of our Dermatophytosis series, Dr. DG Saple discusses two rare case presentations of Tinea, initially misdiagnosed as erythroderma and STD followed by investigations with correct diagnoses and management.
Case 1: Dermatophyte-related erythroderma
A 52-year-old woman presented with complaints of red, raised lesions all over the body with scaling and itching since the past 2 years. (Figure 1a, 1b).

The lesions had initially started over the abdomen and gradually spread to involve the back as well as the upper and lower limbs. She had visited multiple doctors for the same who had prescribed her oral and topical steroids, which would provide temporary relief, but the lesions kept on increasing on stopping the medications.
Investigation
- Cutaneous examination revealed generalised erythroderma and superficial erythematous plaques.
- Her trunk and extremities were predominantly involved. In addition, her fingernails were dystrophic and discoloured.
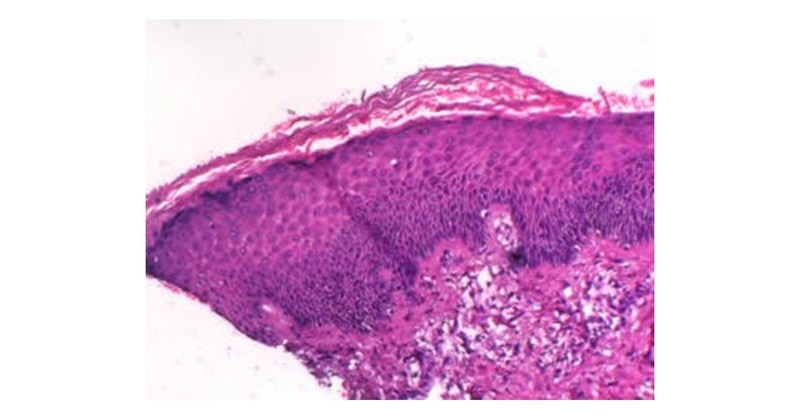
- A skin biopsy was done which showed the presence of fungal hyphae in the stratum corneum. (Fig. 2)
Previously, the patient had been prescribed betamethasone 0.05% cream and triamcinolone 0.1% ointment along with oral methyl prednisolone without improvement.
What is the disgnosis?
Erythroderma or exfoliative dermatitis, presents as diffuse redness and scaling of the skin. There are several causes for erythroderma. However, rarely, Tinea corporis may present as erythroderma.
Treatment
Once the diagnosis of dermatophyte-related erythroderma was made, she received dermatophyte-targeted treatment consisting of oral itraconazole 100 mg twice daily and topical luliconazole cream. The need to be absolutely compliant and adhere to the treatment regimen was impressed onto the patient. She was explained about the need to continue the treatment for atleast 6 to 8 weeks without any interruption. All the steps for personal hygiene were also explained to the patient.
She experienced complete resolution of her erythroderma at the end of 8 weeks (Fig. 3a,3b)

Case 2: Tinea mimicking as an STD
A 68-year-old single male presented with complaints of itchy patches over the groins and over the penis since the past 3 to 4 months. He also complained of occasional burning sensation over the glans penis (Fig. 1).

He did not give a history of lesions anywhere else on the body. He had visited multiple dermatologists before who had prescribed him topical steroidal preparations, oral acyclovir and topical acyclovir ointment, with which he would experience temporary relief. He did not give history of any high-risk behaviour. He was a known diabetic taking oral hypoglycaemic medication.
Investigation
- Clinical examination revealed the presence of erythematous to hyperpigmented plaques in bilateral groins and erythematous papules over the penis topped with erosions.
- PCR test was done to rule out Herpes Simplex Virus (HSV) – I & II, which turned out to be negative.
- A scrapping and KOH mount was performed on the groin plaques and glans, which showed the presence of hyphae in both samples, thus establishing a diagnosis of Tinea cruris and corporis (Fig. 2).
What is the diagnosis?
This patient has a rare case of Tinea with involvement of the penile mucous membrane.
Treatment
The patient was started on oral Itraconazole 100 mg, twice daily – after lunch and after dinner and was counseled regarding strict adherence to the prescribed regimen with proper hygiene care. He was also advised topical Luliconazole 1% cream application twice daily.
However, he developed pedal oedema after starting oral itraconazole, within 2 weeks. Hence, he was shifted to oral terbinafine 250 mg twice daily.
There was a significant reduction in the symptoms after 3 weeks with almost complete resolution of the lesions after 6 weeks, except for PIH (post-inflammatory pigmentation) (Fig. 3).

This article is part of an exclusive series on Dermatophytosis by Dr. DG Saple. Click on the following links to read other articles in the series.
Emerging recalcitrant dermatophytosis in India
Diagnosis of Dermatophytosis- Dr. DG Saple
Resistance in Dermatophytosis- Dr. DG Saple
Tinea cruris & corporis: Current approach and management
Topical antifungals for Tinea infections: What should be prescribed?: Prof. Dr. D.G. Saple
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
The author, Dr. DG Saple is a Senior Consultant and Director of Dermatology at a Mumbai-based clinic.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries