Diagnosis and management of celiac disease – ICMR guidelines
M3 India Newsdesk Jun 28, 2022
Celiac disease is a chronic immune-mediated disease. The ICMR guidelines for clinical presentations, screening methods, diagnosis, management and monitoring of patients with celiac disease are penned down in this article.
Celiac disease is caused by the intake of gluten proteins present in barley, wheat, and rye. The disease mainly affects the small intestine; however, the reproductive system, skin and bone may also be affected.
Clinical presentations
Celiac disease affects each individual differently. It can manifest as an asymptomatic disease to a severe condition.
The term “celiac iceberg” is used to denote the different facets of the disease as only a small proportion of the disease is clinically visible.
- Classical celiac disease – This includes gastrointestinal manifestations such as diarrhoea, malabsorption, weight loss, severe abdominal pain, flatulence and nutrient deficiencies secondary to small bowel mucosal disease. Classical form is observed in children as well as adults.
- Non-classical celiac disease – In this the patients present with non-classical manifestations such as anaemia unresponsive to oral iron therapy, osteoporosis, increase in transaminases, infertility, short stature, bleeding diathesis is usually caused by prothrombin deficiency, neurologic symptoms result from hypocalcemia including paresthesias with sensory loss, motor weakness, and ataxia.
- Asymptomatic celiac disease – This includes healthy individuals who show mucosal abnormalities suggestive of celiac disease but have no symptoms to indicate the presence of celiac disease.
- Potential celiac disease – This group includes individuals who are considered to have the potential to have the celiac disease under the appropriate environmental circumstances but show no mucosal abnormalities or symptoms characteristic of the disease.
Celiac disease if left untreated can lead to severe complications such as
- Refractory CeD
- Celiac crisis
- Ulcerative jejunitis
- Malignancies - Enteropathy T-cell lymphoma, and other malignancies of the small intestine and other parts of the gastrointestinal tract
Serological tests - The first screening tests for celiac disease
Serological tests are the first screening tests. IgA anti-tissue transglutaminase (IgA anti-tTG) is the test of choice to screen individuals with celiac disease.
In patients with strong clinical suspicion of celiac disease, negative serology warrants exclusion of selective IgA deficiency.
In patients with IgA deficiency, an IgG-based test such as IgG anti-tTG Ab or IgG antideamidated peptide Ab may be used.
Mucosal histological changes in celiac disease
Changes in the small intestinal biopsy are the main histology features to identify celiac disease. Villous abnormalities can range from an increase in intra-epithelial lymphocytes [IEL] to marked severe villous abnormality.
1. The biopsy report should be graded as per the modified Marsh Oberhuber classification.
2. The modified Marsh Oberhuber classification of villous abnormalities is used to grade the severity of villous atrophy. The gradings are based on two parameters:
- Increase in IELs
- Villous height to crypt depth ratio
3. Elevated IEL (>30/100 epithelial cells) is not specific to celiac disease and can be present in several conditions such as giardiasis, tropical sprue, and bacterial overgrowth
4. Four to six mucosal biopsies should be obtained from the mucosal folds in the second part of the duodenum and should be oriented well for interpretation
Genetic studies - HLA typing is not required routinely
Individuals with HLA-DQ2/DQ8 haplotypes (homozygous, heterozygous, or compound heterozygous) are particularly susceptible to celiac disease, however, HLA typing is not generally required to diagnose celiac disease.
Who should be screened for celiac disease?
Screening for celiac disease should be carried out in adults or children with:
- Chronic diarrhoea
- Chronic iron deficiency anaemia
- Unexplained short stature
- Failure to thrive in childhood
- Unexplained infertility
- Unexplained osteopenia or osteoporosis
Due to the common genetic background and various environmental and immunological factors, Type 1 diabetes and celiac disease can have significant clinical and pathogenic overlap. Patients with CeD may also be associated with other autoimmune thyroiditis and autoimmune liver disease.
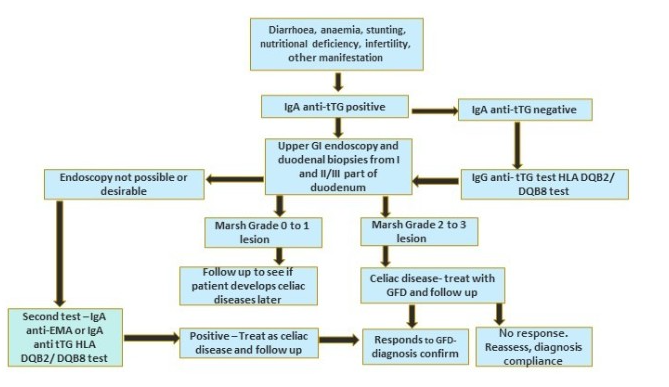
Diagnosing celiac disease
Celiac disease can be diagnosed after considering three parameters:
- Presence of clinical manifestations
- Positive serology
- Presence of villous abnormalities of at least Marsh grade 2 on duodenal biopsy
In cases where duodenal biopsy is not possible, celiac disease can be diagnosed after considering the following parameters:
- Presence of clinical manifestations
- Positive serology of two different kinds such as anti-tTG Ab and a positive anti-endomysial Ab
- Presence of either HLADQ2 or DQ8
Criteria for ‘potential’ celiac disease
- Asymptomatic patients
- Positive celiac serological test
- Villous abnormality of Marsh grade 0 or 1
The diagnosis of celiac disease should not be made based only on a positive celiac serological test irrespective of its titre.
Management of celiac disease
The primary way to manage celiac disease symptoms is lifelong and completely avoiding gluten or gluten-containing dietary items.
- Patients should be counselled for a balanced diet as per their nutritional requirements.
- Patients should receive appropriate nutritional supplementation including vitamin D, calcium, iron, zinc, vitamin B12 and other macro and micronutrients.
- A nutritionist or dietician should be consulted.
- Patients and family including caregivers should be educated regarding the nature and lifelong treatment of the disease
- As exposure to just a small quantity of gluten is sufficient to maintain the disease, a list of restricted and allowed food should be provided.
Monitoring of patients with celiac disease
Patients should be followed up at regular intervals. The following parameters should be evaluated during follow-ups:
- Compliance with a gluten-free diet as most patients respond to a gluten-free diet within weeks to months
- Clinical parameters such as weight, height (for growing age)
- Resolution of symptoms
- Improvement of haemoglobin
Some of the reasons for partial response or non-response include:
- Poor compliance with the dietary restrictions
- Bacterial overgrowth
- Lactose intolerance
- Microscopic colitis
- Parasitic infection
- Refractory celiac disease
Serological tests should be carried out at 6 months and one year to monitor adherence.
Click here to see references
Disclaimer- The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of M3 India.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries