Diabetic Retinopathy: Screening and Management
M3 India Newsdesk Sep 03, 2024
The article explains diabetic retinopathy, emphasising early detection, risk factors, and treatments to prevent vision loss. It also highlights the importance of multidisciplinary care in managing the condition.
Diabetic retinopathy (DR) is a leading cause of “preventable” vision impairment among individuals with diabetes[1], the economic burden of which is considerable in India. It is a microvascular complication of diabetes resulting from prolonged hyperglycemia, wherein the blood vessels in the retina get damaged, leading to vision loss and, in severe cases, even blindness.
Understanding the importance of timely screening and implementing appropriate management strategies is crucial in preventing severe visual outcomes in diabetic people.
The risk factors for DR include duration of diabetes (the most important determining factor), poor control of diabetes (haemoglobin A1c, serum glucose), associated :
- Hypertension (systolic blood pressure)
- Dyslipidemia
- Anaemia
- Smoking
- Obesity and pregnancy
2 After 10 years, approximately 20% of type 1 and 25% of type 2 diabetics develop retinopathy, and after 20 years, almost 80% develop retinopathy.[3]
Pathophysiology of Diabetic Retinopathy (DR)
DR progresses through several stages, each with increasing severity:
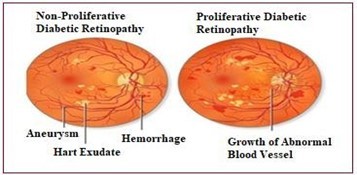
1. Non-Proliferative Diabetic Retinopathy (NPDR)
- NPDR is the early stage of DR and is often asymptomatic. It is characterised by microaneurysms, (saccular dilatations of retinal capillary walls) retinal haemorrhages, and exudates. These changes occur due to damage to the retinal capillaries, leading to increased permeability.
- As NPDR progresses, more blood vessels get blocked, depriving the retina of oxygen (ischemia). This can result in diabetic macular oedema (DME), where fluid leaks into the macula (the central part of the retina responsible for sharp central vision) causing it to swell.
- It is when DME occurs, that the patients become symptomatic (decrease in vision, distorted or wavy vision, altered colour vision). The NPDR progresses through the Mild, Moderate, Severe, and Very Severe stages.
2. Proliferative Diabetic Retinopathy (PDR)
- PDR is the advanced stage of DR and occurs when the retina becomes ischemic. To compensate for the lack of oxygen, the retina starts to grow new, abnormal blood vessels (neovascularisation).
- This occurs secondary to the upregulation of pro-angiogenic factors, mainly the Vascular Endothelial Growth Factor (VEGF).
- The new vessels are fragile and prone to bleeding and thus lead to severe complications such as vitreous haemorrhage (bleeding into the gel-like substance in front of the retina) and tractional retinal detachment (when scar tissue pulls the retina away from the underlying tissue). If left untreated, PDR can lead to complete and irreversible blindness.
Screening for diabetic retinopathy
Early detection is essential to prevent vision loss, as DR is often asymptomatic in its early stages. Screening allows for the identification and treatment of DR before it progresses to a more severe stage. The International Council of Ophthalmology (ICO) and the American Diabetes Association (ADA) provide specific guidelines for DR screening [4].
Type 1 Diabetes: First, a dilated and comprehensive eye examination is recommended within 3-5 years of diagnosis. Since type 1 diabetes typically begins in childhood or adolescence, DR is less common during the first few years after diagnosis, hence the delayed screening.
Type 2 Diabetes: First Retinal exam should be done at the time of diagnosis because DR may be present at the time of diagnosis due to the often insidious onset of type 2 diabetes.
Pregnant Women with Type 1 or 2 Diabetes: Pregnancy can worsen DR, so women with pre-existing diabetes should have a comprehensive (dilated) eye exam soon after conception and in the first trimester, followed by close monitoring throughout pregnancy and the postpartum period.
An eye examination is not required if women without DM newly develop gestational diabetes during pregnancy.
Subsequent screenings should be conducted annually (if no evidence of DR is found and blood sugar levels are well controlled), and more frequently depending upon the severity of DR, at the first exam.
The following methods are commonly used in DR screening
1. Dilated fundus examination
This is the most widely used method and is considered the gold standard for detecting DR. The procedure involves dilating the pupils with eye drops to allow a better view of the retina. An ophthalmologist then examines the retina using a slit lamp and/or an ophthalmoscope, looking for signs of microaneurysms, haemorrhages, exudates, and neovascularisation.
2. Fundus photography
This method involves capturing high-resolution images of the retina. These images can be used for detecting DR, documentation, and monitoring the disease progression.[5] Fundus photography is often used in telemedicine programs, where images are sent to a specialist for evaluation, making it a valuable tool for screening in remote underserved areas, and a cost-effective alternative to examination by an ophthalmologist.[6,7]
3. Optical Coherence Tomography (OCT)
OCT is a non-invasive imaging test that provides cross-sectional images of the retina. It allows for the assessment of retinal thickness and the detection of diabetic macular oedema (DME), even in its early stages. It is particularly useful in cases where macular involvement is suspected.
4. Fluorescein Angiography (FA)
The test involves injecting a fluorescent dye into the bloodstream (ante-cubital vein) to image the blood vessels in the retina. The dye travels to the retinal vessels, and images are taken to identify areas of leakage, ischemia, and neovascularization.[8] FA is typically used when there is a need to assess the severity of DR or guide treatment, particularly laser therapy.

OCT machine
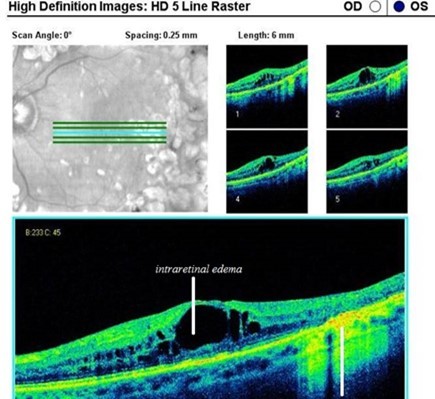
OCT in the case of DME

Dilated fundus examination on slit lamp
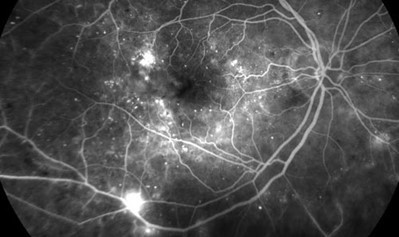
FA in a case of proliferative diabetic retinopathy (PDR)
Management
Management of DR depends on its severity and involves both medical and surgical interventions. The primary goal is to prevent the progression of the disease and preserve vision. Early intervention can significantly reduce the risk of vision loss.
A. Glycemic control: Tight control of blood glucose levels is the cornerstone of preventing and slowing the progression of DR. The ADA recommends maintaining an HbA1c level below 7% to reduce the risk of developing DR or its progression. Studies, such as the Diabetes Control and Complications Trial (DCCT) and the UK Prospective Diabetes Study (UKPDS), have demonstrated that intensive glycemic control reduces the incidence and progression of DR.[9,10]
B. Blood pressure, lipid, and nephropathy control: Medications and lifestyle modifications (such as diet and exercise) to control hypertension and dyslipidemia can reduce the risk of DR progression.[11]
C. Anti-VEGF therapy: VEGF plays a critical role in the development of macular edema and in formation of neovascularisation in PDR. Anti-VEGF agents, such as ranibizumab (Accentrix), bevacizumab (Avastin), and aflibercept (Eylea),[12] are injected into the eye to inhibit the growth of abnormal blood vessels and reduce DME, and are now the standard of care.
D. Intravitreal steroid implants: Long-acting corticosteroid implants like dexamethasone implants (Ozurdex) and fluocinolone acetonide implants (Retisert and Iluvien) are also used in DME. [13] They are reserved for cases not responding to multiple injections of Anti-VEGF medications.
E. Laser photocoagulation: Laser treatment has been used for decades to manage DME and PDR. The procedure involves using a laser to seal leaking blood vessels, reduce macular oedema, and prevent the growth of new blood vessels. There are two main types of laser treatments for DR.
- Focal/grid laser photocoagulation: This is used to treat macular oedema by applying the laser directly to leaking microaneurysms or areas of retinal thickening.
- Panretinal Photocoagulation (PRP): This is used to treat PDR by applying the laser to the peripheral retina. PRP helps to reduce the risk of severe vision loss by causing the abnormal blood vessels to regress and preventing further neovascularization.[14]
F. Vitrectomy: Vitrectomy is a surgical procedure performed in advanced cases of DR, particularly when there is significant vitreous haemorrhage (VH) or tractional retinal detachment (TRD). The procedure involves removing the vitreous gel from the eye and replacing it with saline/air/gas/silicone oil.[15,16] This procedure is also needed for tractional varieties of DME.

Intravitreal injection

ANTI-VEGF agents
 Steroid implant
Steroid implant

Retinal laser photocoagulation
Emerging therapies and future directions
Research into new treatments for DR is ongoing, with several promising approaches being explored. These include:
- Gene therapy: Researchers are investigating the potential of gene therapy to treat or prevent DR by targeting specific genes involved in the disease process.
- Neuroprotective agents: These agents aim to protect the retinal neurons from damage due to hyperglycemia and other metabolic changes associated with diabetes.
- Artificial Intelligence (AI) in DR screening: AI-based algorithms are being developed to assist in the early detection of DR by analysing retinal images.[17] These tools could help increase access to screening, particularly in underserved areas.
Conclusion
- Educating patients about the importance of regular eye exams (timely screening) and maintaining good metabolic control is vital.
- Patients should be informed about the symptoms of DR, such as blurred vision, distorted vision, floaters and sudden vision loss, and encouraged to seek immediate medical attention whenever needed.
- Regular follow-up with an ophthalmologist is essential to monitor the progression of DR and adjust treatment as needed. With the advent of new technologies and treatments, the future looks promising for improving outcomes in patients with DR.
- Collaboration between healthcare providers, including primary care physicians, endocrinologists, nephrologists and ophthalmologists, is essential in managing this condition effectively and ensuring that patients receive the best possible care.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Charu Malik is MS, DNB, FNB- vitreoretinal surgery, working as Assistant Professor of Ophthalmology and VitreoRetina Consultant at SMS&R, Sharda Hospital, Sharda University, G. Noida, and Consultant Ophthalmology at Jaypee Hospital, Noida.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries