Crucial Signs of Respiratory Tract Infections
M3 India Newsdesk Jan 06, 2024
This article discusses the crucial signs & symptoms of respiratory tract infections, emphasising the importance of thorough patient history for accurate diagnosis. It provides guidance on patient evaluation, management, and when to consider antibiotic prescriptions, referencing NICE guidelines.
RTIs (respiratory tract infections) are a common condition seen by general practitioners (GPs). Antibiotic prescriptions are often made for a variety of reasons. A small RTI might potentially be something more serious. A thorough history is crucial to avoid missing a dangerous diagnosis in these typical presentations.
This article deals with a compilation of indicators that raise concerns regarding infections of the respiratory tract, encompassing potential aetiologies, pertinent inquiries, and recommended diagnostic procedures.
Warning signs and symptoms
The following symptoms may persist longer than three weeks:
- Hemoptysis
- Persistent hoarseness
- Persistent sore throat
- Persistent unilateral enlarged tonsil
- Difficulty finishing sentences
- Difficulty swallowing (especially own saliva)
- Shortness of breath
- Pleuritic chest pain
- Headache, photophobia, and stiff neck
- Non-blanching rash
- Nasal flaring/grunting in babies
- Regression of intercostal muscles in young children and babies (>3 weeks)
- Symptoms not alleviated by conventional treatments
- History of Overseas Travel
How the patient presents
It's critical to comprehend the patient's goals, thoughts, worries, and aspirations, as well as the reason for their current presentation.
Knowing what patients are looking for is vital since not all patients will need antibiotics; in some cases, reassurance may work just as well.
Certain patients, who suffer from long-term respiratory conditions including COPD, asthma, or bronchiectasis, will see a physician to rule out a potential bacterial infection.
Adult RTIs may manifest in a variety of ways. Patients may complain:
- "I have trouble sleeping; it's this cough."
- "I've been producing phlegm."
- "It hurts to speak."
- "I believe I have a cold."
- "It's my chest again."
- "I feel like I'm chesty."
These are the typical situations. Nevertheless, additional symptoms could manifest as dyspnea or pleuritic chest discomfort, which is pain during deep breathing and/or coughing.
Finding out how long the presenting ailment has been present is the first step.
- Are there any further concomitant symptoms?
- Does the patient have a bad feeling?
- Do they have a temperature?
Further testing might be necessary if the patient complained of being out of breath. It might be useful to evaluate their tolerance to exercise and investigate how dyspnea is affecting their ability to do everyday tasks. Is the dyspnea worse than it was the day before?
Additionally, you may want to inquire if any ankle oedema, orthopnea, or paroxysmal nocturnal dyspnea are present.
Inquiries about swallowing problems, eating and drinking issues, and a history of swollen glands should be made in response to a sore throat.
The following are other aetiologies that might account for symptoms of the respiratory tract:
Infectious causes:
- COVID-19
- Infections
- Pneumonia
- Bronchiolitis
- Exacerbations of long-term lung problems
- HIV
- Peritonsillar abscess (quinsy)
- Pharyngitis
- Tracheitis
- Tuberculosis
- Influenza
Non-infectious causes:
- Asthma
- Bronchiectasis (may cause recurring lower respiratory tract infections)
- Bronchogenic cancer
- COPD (Chronic Obstructive Pulmonary Disease)
- Heart failure
- Sarcoidosis
- Tonsillar malignancy
- Pulmonary embolism
- Pulmonary fibrosis
- Interstitial lung disease
Adult evaluation and management
Reflux and lifestyle factors:
Given the length of the symptoms, it might be pertinent to inquire about reflux symptoms and to get a thorough history of alcohol and tobacco use.
Cough-related inquiries:
Inquiries about expectoration, hemoptysis, chest discomfort, weight loss, and dyspnea should be made in response to a cough.
Smoking history significance:
When determining a potential differential diagnosis, the smoking history may be crucial. If you have any suspicions regarding TB or HIV, you may want to inquire about foreign travel or the patient's history of sexual activity.
Exploring non-respiratory causes of cough:
A persistent cough presents many non-respiratory options. Heart failure, medications (such as ACE inhibitors), and gastro-oesophageal reflux disease are among the possible causes.
Sinusitis consideration:
Asking about potential sinusitis when there is a history of face discomfort, fever, post-nasal drip, headache, or diplopia may be prompted by nasal congestion.
Impact of chronic illness:
A history of one or more chronic illnesses may alter the available treatments.
Medication and immunosuppressant assessment:
In order to determine if the patient is taking any drugs that might be affecting their presentation, such as immunosuppressants, a thorough drug history is necessary.
Paediatric evaluation and treatment
Key areas of focus:
The evaluation for children will be different, with extra questions centred around eating, respiratory rate, irritability, urine output, and the existence of a non-blanching rash.
Vaccination schedule and delivery history:
When it comes to children, it's important to find out whether the vaccination schedule is current and if the delivery was problematic.
Fever monitoring and referral indicators:
If the kid develops a fever, watch out for symptoms that could need an immediate referral. For the purpose of determining the risk of severe disease in children under five, the NICE traffic light scoring system may be helpful.
Comprehensive paediatric examination:
A paediatric examination will include monitoring the child's overall health as well as watching the child's chest, breathing rate, capillary refill time, and appearance of signs of pyrexia. An ENT examination will probably be required as well. Take a child's oxygen saturation levels into consideration.
Remote evaluation
When evaluating patients over the phone, consider the following:
- What is the patient's voice like?
Is there a wheeze audible?
- Are they able to finish sentences?
- Can they measure their oxygen saturation with a pulse oximeter?
When evaluating patients via video, consider the following:
- How does the patient appear?
- Has the rate of respiration increased?
- Is central cyanosis evident in any way?
- Are they able to finish sentences?
- Is breathing with pursed lips present?
In-person evaluation
Vital signs monitoring:
Temperature, pulse, oxygen saturation, and respiration rate should all be checked throughout the examination.
Blood pressure consideration:
Blood pressure could or might not matter.
Speech difficulty assessment:
Does it become hard to finish sentences?
Pharynx and tonsil examination:
Look closely at the tonsils while you examine the pharynx. Are they here? If yes, are they proportionally enlarged? Does anything exude? Is there any proof that quinsy exists?
Lymph node palpation:
It could be required to palpate lymph nodes, with special attention to the submental, submandibular, and cervical chains.
Sinus examination:
It could be required to palpate the sinuses and look for nystagmus if sinusitis is suspected.
Neurological assessment:
Is meningism suspected or proven?
Cardiovascular auscultation:
To determine the heart rate, auscultate the lung areas while keeping an ear out for any new noises or heartbeats.
Exams and history will serve as the foundation for the investigations. But the majority of GPs will have access to:
- Blood tests:
- Full Blood Count (FBC)
- C-reactive protein (CRP)
- NT-proBNP (N-terminal pro-B-type natriuretic peptide)
- Imaging:
- Plain Chest X-ray
- Cardiac assessments:
- Electrocardiogram (ECG)
- Echocardiogram
- Respiratory tests:
- Sputum Culture and Sensitivity
- Pulmonary function assessment:
- Pulmonary Function Tests
Fast admission and recommendation
Unstable heart rate:
In the event that the patient's heart rate is unstable, consider an immediate admission.
Concerns of malignancy or abnormal chest x-ray:
In cases where malignancy or abnormal chest X-ray results are concerns, take into consideration the two-week wait (2ww) approach.
Lack of response to standard therapies or concerns about chronic pathology:
If the patient is not responding to standard therapies or if there are concerns about a more chronic respiratory or cardiac pathology, take counsel, guidance, and/or referral into consideration.
When to provide antibiotic prescriptions
The use of antibiotics in primary care is closely monitored. It is believed that the majority of RTIs resolve on their own and don't need to be treated with antibiotics.
While prescribing antibiotics to patients who come with acute pharyngitis, consider the FeverPAIN score or the Centor criteria.
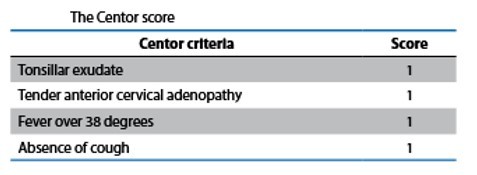
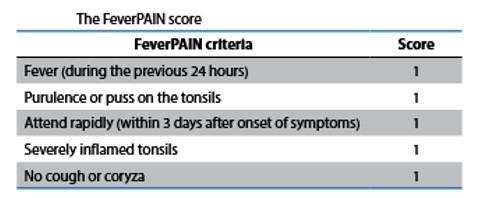
A FeverPAIN score of 0 or 1, or a Centor score of 0, 1, or 2, indicates that the patient is not likely to benefit from antibiotics or a throat culture.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Monish Raut is a practising super specialist from New Delhi.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries