Clinical Presentation of Gallbladder Stones and its Management
M3 India Newsdesk Nov 07, 2023
This article discusses the prevalence of gallstones and the clinical presentations of gallstone-related diseases. It also provides a case study illustrating the diagnosis and treatment of acute calculous cholecystitis, following the Tokyo guidelines.
The reported prevalence in India is around 6.1% (men 3.1% and women 9.6%). The prevalence of gallstones increases with age. At the age of 65, about 30% of women have gallstones, and by the age of 80, 60% of both males and females have gallstones.
Patients with gallstone disease are mostly diagnosed incidentally or present with a myriad of symptoms, which often overlap with other organic and functional GI disorders.
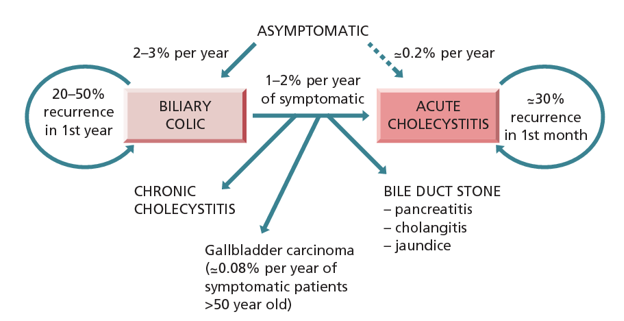
Making an accurate diagnosis of gallstone-related diseases or their complications is important because, with each passing attack of biliary colic, the chances of complications increase. Hence, a clear understanding of various clinical presentations and the management of gallstones is crucial for physicians and surgeons to provide effective care for their patients.
These case vignettes illustrate the diverse clinical presentations and management strategies associated with cholelithiasis.
Case1
A 55-year-old female presented for a routine health checkup. She had no significant medical history and was not experiencing any specific symptoms. During a health check-up, an ultrasound showed gallstones.
What is the natural history of asymptomatic gallstones?
With the increasing use of ultrasound for various clinical indications; incidental detection of gallstones is persistent. This case illustrates a dilemma frequently encountered in everyday clinical practice.
Long-term follow-up studies from the West have consistently shown that only a small minority of asymptomatic gallstones lead to the development of symptoms or complications.
What are the treatment options for gallstones?
- Oral dissolution therapy is usually minimally successful. It only works for cholesterol gallstones if the size is less than 6 mm.
- Knowing gallstone composition based on imaging alone is not possible. It also needs the use of medications for several months and stones often recur after cessation of medications. Hence it is only used in uncomplicated and only mildly symptomatic patients who either refuse or cannot undergo surgery.
- Laparoscopic cholecystectomy remains the surgical choice.
Considering the fact that in most cases, gallstones will remain asymptomatic, should you treat asymptomatic gallstones?
- This group of patients is asymptomatic, yet they are nevertheless at lifelong risk of symptoms and problems. However, laparoscopic cholecystectomy also carries risks associated with anaesthesia and iatrogenic complications (mortality of 0.22-0.4%, major morbidity of 5%). Considering the balance of risks; the current standard practice is to recommend cholecystectomy only for symptomatic patients.
- At the same time, there is a general agreement on early prophylactic cholecystectomy in selected groups of patients such as those with chronic hemolytic syndromes. These patients have been shown to be at a higher risk of developing symptoms and complications.
- Additionally, people have advocated cholecystectomy in patients originating from areas of endemic gallbladder cancer (eg, Gangetic plains of North India), diabetics, transplant recipients and incidental peri-operative discovery.
- However, due to gaps in current knowledge, the clear division of patients into low or high-risk gallstone-related complications is still far from ideal and hence their management is controversial.
Case 2
A 45-year-old woman presents to the casualty with persistent, severe right upper abdominal pain and vomiting. She also has pain around her right scapula. The pain began 6-7 hours prior, and there are no clear precipitating factors. However, she does recall having intermittent, less severe episodes of abdominal discomfort over the previous year.
She states that using antacids does not relieve her chronic pain, which flares up after hefty meals and disappears on its own. She has a history of obesity and diabetes. She rejects experiencing dizziness, heartburn, lower stomach pain, or chest pain.
Her examination findings include:
- Blood pressure -125/88
- Heart rate - 117
- Respiratory rate - 16
- Temperature - 98.9 F
The abdominal examination reveals marked tenderness to palpation in the right upper quadrant (RUQ) and a positive Murphy’s sign (RUQ pain with inspiration during deep palpation, just below the ribs).
Based on history, what is the differential diagnosis, and what further testing is warranted?
- The character and timing of this patient’s pain is consistent with biliary colic.
- The phrase biliary colic—suggesting fluctuating pain in nature—appears ubiquitously in the medical literature, but it does not correctly characterise the pain associated with gallstones.
- Biliary colic usually has a crescendo-decrescendo pattern, with the pain slowly building up to a peak during a few hours; this peak is often associated with vomiting, and the pain then gradually subsides during the ensuing few hours.
- Pain often remits spontaneously after several hours, leaving some residual soreness in the right upper quadrant, usually due to an element of “chemical” cholecystitis.
- Gallbladder nociceptors are assumed to be the source of this pattern of gallbladder pain, which occurs in reaction to an increase in intracholecystic pressure brought on by the gallbladder contracting forcefully against an obstruction in the neck.
- The frequency of these pain episodes can vary greatly; some individuals may have years between episodes, while others may experience near-constant suffering.
- More than 60% of patients will suffer recurrent pain within 2 years of their initial attack, and several studies have indicated that gallstone-associated complications occur more frequently in patients who experience biliary colic.
- If pain persists beyond 6 hours, as in this case, it can herald a worse complication of gallstones, such as cholecystitis, cholangitis, or pancreatitis.
Other diagnoses
- Other diagnoses that could be investigated are angina, myocardial infarction, peptic ulcer disease, gastroesophageal reflux disease, pancreatitis, and other diseases leading to acute hepatic congestion.
- This patient did not report angina discomfort, which is typically sudden, acute, in the chest, and associated with effort. Although myocardial infarction might present with unusual symptoms, this patient did not have the classic chest pressure or crushing sensation, nor did she have radiation to the arm or jaw.
- Antacids are usually used to treat stomach pain brought on by gastric acid production during meals; however, this patient did not have this condition. Heartburn is related to irritation of the lower oesophagus by gastric acid, which also was relieved by antacids.
- Diagnostic tests and procedures should be ordered to evaluate each of these diagnoses further if clinical suspicion exists (ie, electrocardiogram and troponins for myocardial infarction, endoscopy for peptic ulcer disease, amylase and lipase for pancreatitis, liver enzymes for hepatobiliary disease). However, the most likely diagnosis in this case is acute calculous cholecystitis.
- In this case, testing focused on gallbladder disease was pursued because of characteristic clinical presentation, and lack of symptoms supportive of another aetiology.
- Blood count, CRP and routine blood biochemical tests including LFT were obtained. Additional special tests such as serum pancreatic enzyme estimation were done. Her total leukocyte count was 14,300 /cumm, and CRP was 27 mg/mL. Other biochemical tests were within normal limits.
- Ultrasound abdomen showed multiple, gallbladder calculi, thickened GB wall and pericholcystic fluid.
According to Tokyo guidelines, the patient was diagnosed with mild acute calculous cholecystitis based on clinical findings, supportive laboratory findings and characteristic radiological findings.

According to recommendations in Tokyo guidelines, laparoscopic cholecystectomy was performed in the same admission. Intra-op findings included - an intact inflamed gallbladder without evidence of local complications.
During the follow-up visit, the patient was doing well clinically. The histopathology report showed changes suggestive of acute or chronic cholecystitis.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Parag Dashatwar is a DNB gastroenterologist, who leads the department of medical gastroenterology at Olive Hospital, Hyderabad
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries