Chronic Urticaria and Treatment Protocols
M3 India Newsdesk Jun 07, 2023
Chronic urticaria is a dermatologic condition characterised by recurrent pruritic wheals and angioedema. In this article, read about the different types and management of this condition.
Case presentation
Patient history
A 35-year-old female presented with a history of recurrent pruritic wheals and angioedema over the last six months. She had initially sought treatment from a dermatologist and was diagnosed with CU following a positive autologous serum skin test (ASST). She was started on strong topical corticosteroids and oral antihistamines but had minimal relief, and the symptoms persisted.
Evaluation
The patient was referred to an immunologist for further evaluation and management. Total serum IgE levels were elevated, and an autoimmune workup revealed positive ANA and anti-TPO antibodies, suggestive of an autoimmune aetiology for CU confirmed by a second positive ASST.
Stepwise approach to treatment
After a multidisciplinary team consultation, the patient was started on a stepwise approach, including first-generation H1 antihistamines in combination with H2 antihistamines (cetirizine and ranitidine) and oral corticosteroids. Due to inadequate symptom relief, the patient’s therapy was escalated to the addition of omalizumab, a monoclonal anti-IgE antibody, resulting in a significant improvement in symptoms.
Introduction
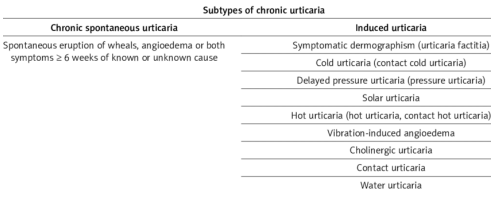
Chronic urticaria (CU) is a commonly occurring dermatologic condition characterised by the recurring presence of wheals and/or angioedema for more than six weeks. The causes for CU are many and could include autoimmune, infectious, medication or environmental factors. In a significant proportion of cases, underlying causes are not detected. The condition can significantly impact the quality of life of affected individuals, but effective treatment options are available.
Pathogenesis of chronic urticaria

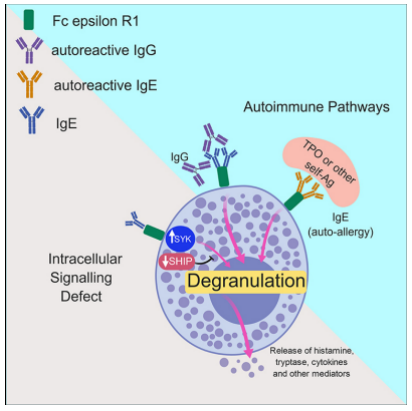
Urticaria results from the release of histamine, bradykinin, kallikrein, and other vasoactive substances from mast cells and basophils in the superficial dermis, resulting in intradermal oedema caused by capillary and venous vasodilation and occasionally caused by leukocyte infiltration.
Types of chronic urticaria
Autologous serum skin testing
Autologous serum skin testing is an investigative test for chronic urticaria.IgE antibodies, known as immunoglobulin-E, play a role in activating receptors called FceRI on mast cells and basophils. These cells are responsible for releasing histamine, a crucial mediator in allergic reactions. In the case of autoimmune urticaria, the condition arises from autoantibodies that bind to either the FceRI receptors or the IgE antibodies directly. This causes inappropriate activation of the mast cells and basophils and the release of histamine.
Autologous serum skin testing is utilised to identify the presence of circulating autoantibodies, indicating an autoimmune source in certain individuals experiencing chronic urticaria.
Benefits
Autologous serum skin testing is relatively reliable, with a sensitivity of 70% and a specificity of 80%. It is inexpensive and straightforward to administer.
Disadvantages
It is important for autologous serum skin testing to be performed by a skilled practitioner, as an inadequate technique can result in misleading outcomes, either producing false positive or false-negative results.
Autologous serum skin testing lacks standardisation, as the literature describes various methods and different criteria that exist for defining a positive outcome.
Positive results may occur in patients that do not have chronic urticaria, for example:
- Patients with autoimmune thyroid disease
- Up to 80% of children with allergic or non-allergic respiratory symptoms
- Drugs such as antihistamines, corticosteroids and immunosuppressant medications
Although a positive autologous serum skin test may indicate autoimmune urticaria, it does not reflect the severity of the disease.
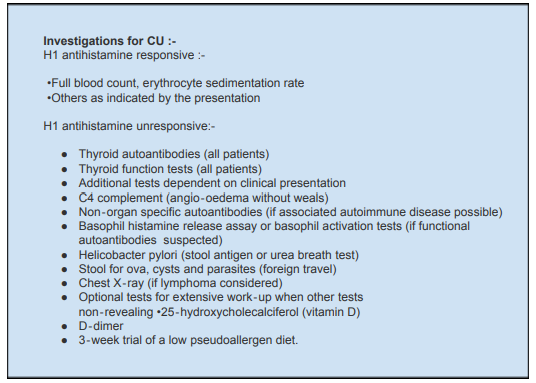
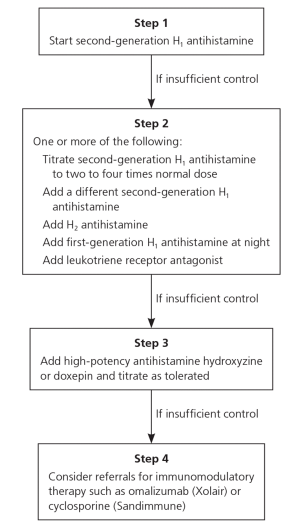
Management and discussion
The treatment of CU is complex, and a multidisciplinary approach is recommended. The aim of treatment is complete symptom control and to improve the overall quality of life of affected individuals. As a first-line therapy, second-generation H1 antihistamines are recommended, with the dosage increased above standard dosing if symptoms persist. The current guidelines suggest adding first-generation H1 antihistamines or H2 antihistamines if the second-generation antihistamines have not provided complete relief.
In cases where conventional therapy has not provided sufficient symptom relief or the disease is severe, third-line therapies are recommended. This includes the use of immunomodulatory agents, such as oral corticosteroids, cyclosporine, or omalizumab. The use of these drugs needs close monitoring due to the incidence of adverse drug reactions.
Conclusion
CU is a complex and challenging disorder that requires a multidisciplinary approach. The underlying causes for the condition are often not identified. Standard evaluation and treatment options are recommended before opting for immunomodulatory agents. The current guidelines provide multiple options in the management of CU, but the choice of therapy should be individualised based on the severity of the disease and the patient’s response to treatment.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Monica Gundecha is an MD (skin & VD) from Pune.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries