Managing Chronic Kidney Disease
M3 India Newsdesk Nov 08, 2024
This article outlines evidence-based dietary guidelines for managing CKD in the Indian population. It explains that effective dietary interventions can slow disease progression, enhance patient outcomes, and delay the need for dialysis.
Chronic Kidney Disease (CKD) affects millions of individuals worldwide, including a significant portion of the Indian population. With its progressive nature, CKD can ultimately lead to end-stage renal disease, requiring dialysis or kidney transplantation. However, effective nutritional interventions can slow CKD progression, improve patient outcomes, and delay the need for dialysis.
This article presents evidence-based dietary guidelines that doctors can incorporate into managing CKD patients, specifically focusing on the Indian population.
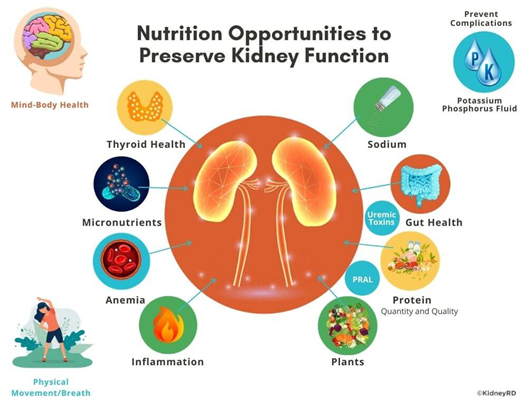
The role of nutrition in CKD progression
CKD is characterised by the gradual decline in kidney function, affecting the kidneys' ability to filter waste, maintain electrolyte balance, and regulate blood pressure. Nutritional management is essential to prevent complications like hyperkalemia, hyperphosphatemia, and fluid overload. The primary goals of dietary intervention are:
- Control of protein intake: To reduce the load on the kidneys and minimise uremic toxins.
- Management of electrolytes: Particularly potassium, sodium, and phosphorus.
- Prevention of malnutrition: Due to restrictive diets and altered appetite in CKD patients.
- Fluid management: To prevent fluid overload and hypertension.
- Control of blood sugar and blood pressure: In patients with underlying diabetes and hypertension, which are major contributors to CKD.

1. Protein restriction: Quality over quantity
A key component of CKD management is protein control, especially in non-dialysis patients. Protein metabolism generates nitrogenous waste, which is excreted by the kidneys. When kidney function is compromised, excessive protein intake can accelerate the accumulation of waste products, worsening uremia.
- Recommended protein intake for non-dialysis CKD patients: 0.6-0.8 g/kg/day: This means that a patient weighing 60 kg should consume between 36-48 g of protein per day.
- Recommended protein intake for dialysis patients: Once dialysis is initiated, protein needs increase due to losses during treatment. The recommended intake is 1.2 g/kg/day for hemodialysis patients.
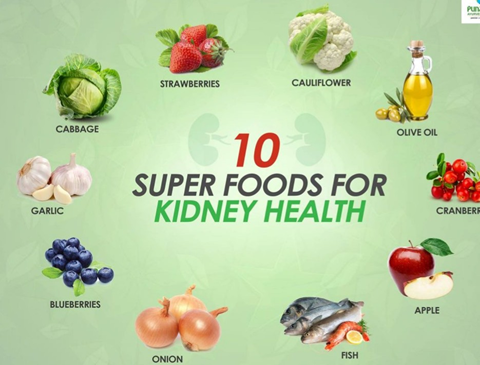
- Sources of high-quality protein: Eggs, fish, lean poultry, and plant-based proteins like lentils and soy. For the Indian population, vegetarian protein sources like paneer and moong dal can be emphasised, though in controlled amounts.
2. Potassium management
In CKD, the kidney's ability to excrete potassium diminishes, leading to hyperkalemia. Elevated potassium levels can cause dangerous heart rhythms and muscle weakness, making it critical to manage potassium intake in advanced CKD.
- Recommended potassium intake: Typically restricted to 2,000-2,500 mg/day for patients with hyperkalemia.
- High-potassium foods to avoid: Bananas, oranges, tomatoes, potatoes, and spinach.
- Low-potassium alternatives: Apples, berries, radish, cauliflower, and cabbage, which are commonly consumed in the Indian diet.
3. Phosphorus control
Excess phosphorus in the blood leads to vascular calcification and bone disorders in CKD patients. Since the kidneys can no longer efficiently excrete phosphorus, managing dietary intake is crucial.
- Recommended phosphorus intake: 800-1,000 mg/day
Phosphorus is found in dairy products, processed foods, and certain meats. Reducing the intake of packaged foods and focusing on fresh, homemade meals can help manage phosphorus levels. Indian foods like Jowar bhakri/ roti, a type of flatbread, and vegetables like bottle gourd can be encouraged over processed snacks.
4. Sodium and fluid restrictions
Sodium management is essential for controlling blood pressure and preventing fluid overload in CKD patients. Excess sodium leads to water retention, worsening hypertension and heart failure risk.
Recommended sodium intake: 2,000 mg/day, or less than 5 grams of salt per day.
Fluid management: For patients with fluid retention, fluid intake may be restricted based on urine output and dialysis status. Fluid intake should be individualised but typically falls between 1,000-1,500 mL/day, including water, tea, and other liquids.
For Indian patients, cutting back on high-sodium pickles, papads, and processed snacks like farsan/ namkeens is important. Instead, using fresh herbs and spices for flavour can help manage sodium intake.
5. Caloric intake and micronutrients
Caloric intake should be sufficient to prevent muscle wasting and malnutrition, a common issue in CKD patients, particularly those on restrictive diets. It is important to ensure that CKD patients, especially vegetarians, receive enough calories from carbohydrate and fat sources.
Recommended caloric intake: 30-35 kcal/kg/day depending on activity level and nutritional status.
Micronutrient supplementation may be necessary, particularly for vitamin D and iron. As the kidneys lose the ability to activate vitamin D, supplementation with calcitriol can help manage bone health. Additionally, iron supplementation may be required to manage CKD-related anaemia, along with erythropoiesis-stimulating agents (ESAs).
Practical considerations for the Indian population
Given regional dietary preferences and cultural practices, it is essential to adapt CKD dietary recommendations to suit the Indian context:
- Vegetarian protein sources: Encourage legumes, pulses, and paneer while balancing phosphorus and potassium intake.
- Spice usage: Use low-sodium spice blends like jeera, turmeric, and coriander to flavour dishes while avoiding excessive salt.
- Fluid management: Advise patients to control their intake of liquids, including traditional beverages like buttermilk and coconut water, depending on their fluid status.
Case study 1
Protein restriction in pre-dialysis CKD
A 50-year-old male with Stage 3 CKD, secondary to diabetes, presents with proteinuria and a declining GFR of 45 mL/min. His daily protein intake exceeds 90 g. After reducing his protein intake to 0.6 g/kg/day (42 g/day) and focusing on plant-based sources, his eGFR stabilises, and proteinuria decreases. Blood pressure and glucose levels remain controlled.
Key takeaway: Early intervention through protein restriction can help prevent CKD progression in non-dialysis patients.
Case study 2
Potassium and phosphorus management in dialysis
A 65-year-old female on hemodialysis presents with elevated phosphorus (6.2 mg/dL) and potassium levels (5.9 mEq/L). Her diet reveals excessive consumption of high-potassium foods like bananas and high-phosphorus dairy products. After reducing these foods and initiating phosphate binders, her levels return to target within two months.
Key takeaway: Effective electrolyte management can prevent complications in CKD patients, particularly those on dialysis.
Conclusion
Nutritional management in CKD is essential for delaying disease progression and improving patient quality of life. By providing individualised, evidence-based dietary advice, physicians can help their patients manage protein, electrolyte, and fluid intake more effectively. Tailoring recommendations to suit cultural and regional dietary habits, such as those in the Indian population, can further enhance adherence and outcomes.
The integration of nutritional strategies into CKD management, coupled with ongoing monitoring and patient education, is critical for the long-term success of CKD treatment.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
The author of this article: Ms Rutambhara Nhawkar is a Clinical Dietician, M. Sc. (Clinical Nutrition & Dietetics), Certified Diabetes Educator and a medical writer from Pune.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries