Changing the Way Type 2 Diabetes is Treated in Primary Care
M3 India Newsdesk May 26, 2023
This article highlights the role of sodium-glucose cotransporter 2 (SGLT2) inhibitors & glucagon-like peptide 1 (GLP-1) receptor agonists in managing glycemic control and cardiorenal risk. The updated guidelines and reframes of doctors' approaches to diabetes pharmacotherapy are also discussed here.
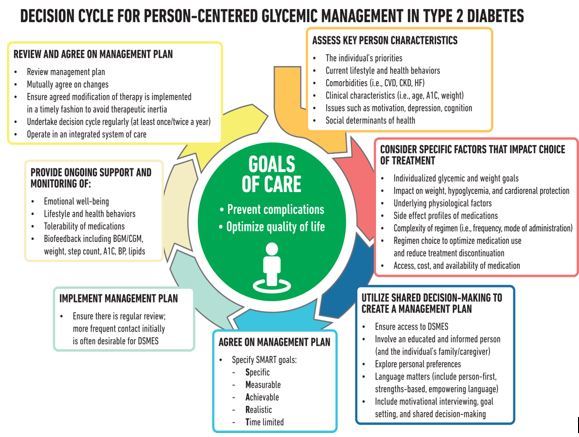
The majority of type 2 diabetes (T2D) patients are managed by family physicians. As a result, family physicians are in a unique position to help T2D patients with glycemic management and cardiometabolic health.
Recently, the landscape of diabetes management has changed from being glucocentric to concurrently focusing on glucose management and cardiometabolic risk due to new information on the roles of sodium-glucose cotransporter 2 (SGLT2) inhibitors and glucagon-like peptide 1 (GLP-1) receptor agonists in glycemic management and cardiorenal risk reduction.
Recent revisions to the American Diabetes Association's Standards of Care in Diabetes guideline, especially those concerning the use of SGLT2 inhibitors and GLP-1 receptor agonists, call for family physicians to reframe approaches to diabetes pharmacotherapy and inform patients of the significance of managing cardiorenal and metabolic risk in addition to blood sugar levels.
Primary Care Physicians (PCPs) are at the forefront of this disease's therapy, making it more crucial than ever for them to be informed on the most recent guidelines as they adapt their practices to assist patients in achieving better cardiometabolic health.
Management of diabetes: Toward a new paradigm
In addition to concentrating on glucose control and the prevention and treatment of microvascular and macrovascular problems using non-glucose lowering medications, the new paradigm of diabetes therapy stresses cardiorenal risk reduction and weight management.
While statins, ACE inhibitors, and angiotensin receptor blockers (ARBs), among other non-glucose lowering medications, have long been prescribed to prevent and reduce the risk of cardiorenal disease, evidence-driven revisions to the Standards of Care in Diabetes now suggest the prescribing of diabetes medications to manage cardiorenal risk regardless of glycemic control.
- For type 2 diabetics who also suffer from heart failure (either preserved or decreased ejection fraction) and chronic renal disease, SGLT2 inhibitors are considered first-line therapy. Similarly, for patients with or at risk for atherosclerotic cardiovascular disease (ASCVD), either a GLP-1 receptor agonist or an SGLT2 inhibitor with demonstrated cardiovascular benefit is recommended.
- If extra glycemic control or risk-factor reduction is required for individuals who have indications for both SGLT2 inhibitors and GLP-1 receptor agonists, the inclusion of the alternative drug is advised.
The American Diabetes Association's Standards of Care in Diabetes, which include a condensed version for primary care physicians that also highlights important updates each year, summarises evidence-based guidelines for comprehensive management of diabetes, cardiometabolic risk, and complications related to diabetes. These recommendations are updated annually.
The US Food and Drug Administration (FDA) required long-term cardiovascular outcome studies with evidence to exclude an elevated risk for serious adverse cardiovascular events for all novel glucose-lowering medicines in 2008. Since that time, several studies have shown the cardiovascular safety and glycemic effectiveness of dipeptidyl peptidase (DPP-4) inhibitors, SGLT2 inhibitors, and GLP-1 receptor agonists.
Many SGLT2 inhibitors and GLP-1 receptor agonists showed cardiovascular benefit in these studies, which was an unexpected discovery. The family physician's approach to managing diabetes has changed as a result of subsequent research that consistently showed improvements in heart failure, coronary artery disease, and chronic kidney disease.
Rethinking pharmacotherapy
- The unanticipated advantages of SGLT2 inhibitors and GLP-1 receptor agonists for the cardiovascular system are also changing how the diabetic medication is approached. For many years, glycemic control as assessed by the HbA1c has been the main focus of diabetes care.
- The most popular first-line drug in this paradigm is metformin, with other medications given as necessary to reach glycemic objectives. There is no need to continue stepping up diabetes treatment after glycemic control has been attained.
- The cornerstone of diabetes therapy for many years has been this approach to glucose control, together with the screening and management of microvascular problems and the treatment of hypertension and cholesterol to guideline-recommended levels to lower the risk for macrovascular consequences.
- This strategy has been further supported by diabetes quality indicators that direct clinical treatment by informing patients about their glucose control and risk for complications.
- It takes tremendous cognitive restructuring on the part of family physicians to prescribe a diabetic medication when a patient's glycemic control is "at target" and to include patients in treatment choices. However, taking this step may not be as difficult as it first seems.
- The 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults led to a similar change in treatment approach. In order to reach a target low-density lipoprotein (LDL) cholesterol objective based on coronary heart disease risk category (low, moderate, and high), the Adult Treatment Panel III (ATP III) recommendations advised a treat-to-target method prior to 2013.
- The 2013 ACC/AHA recommendation recommended fixed-dose statin medication, with dosage intensity adjusted by patient risk, as opposed to cholesterol management based on LDL treatment objectives.
- This modification had a major effect on cholesterol management in primary care, combined with decreasing the 10-year risk threshold to commence statins for primary prevention of ASCVD to 7.5%. Clinicians had previously recommended statins based on LDL levels, but they now had to expand the scope of their approach to managing ASCVD risk.
- As a consequence, many patients with previously regarded "at goal" LDL values now satisfy guideline criteria for statins for primary prevention or are receiving new recommendations for statin intensification.

Pursuing efforts to enhance outcomes
There is a significant potential to enhance cardiovascular and renal outcomes in T2D patients as PCPs attempt to modify their approach to managing diabetes and adapt to the new treatment paradigm.
- PCPs write more prescriptions for SGLT2 inhibitors and GLP-1 receptor agonists than any other physician, even though only 12%–14% of patients who qualify for these treatments get the recommended care.
- Additionally, in the absence of symptomatic hyperglycemia or indications of continuing catabolism, GLP-1 receptor agonists are increasingly preferable.
- The preference for GLP-1 receptor agonists reduces the risk of hypoglycemia and shows a stronger emphasis on weight management as a crucial aspect of diabetes therapy. Greater than 10% weight reduction has the potential to enhance long-term cardiovascular outcomes and has the potential to change disease.
- Although SGLT2 inhibitors and GLP-1 receptor agonists are recommended by guidelines, high out-of-pocket expenses continue to be major roadblocks to prescription and adherence.
- There are currently no generic formulations of SGLT2 inhibitors or GLP-1 receptor agonists. However, in the next few years, generic versions of liraglutide and dapagliflozin could be accessible. Clinicians and patients will continue to depend on prescription discount cards and other programs offered by pharmaceutical firms up to that time.
- Healthcare professionals may assist patients with T2D in achieving their weight reduction objectives by prescription of GLP-1 receptor agonists that are recommended by guidelines, regardless of glycemic control. We can take advantage of the mortality advantages of SGLT2 inhibitors and GLP-1 receptor agonists that may help patients live longer by lowering the risk of CVD & chronic renal disease when we prescribe statins for secondary prevention of cardiovascular disease.
- It is possible to add SGLT2 inhibitors to the patient's heart failure regimen in an attempt to keep them out of the hospital as we study guideline-directed medical treatment in patients with heart failure.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Monish Raut is a practising super specialist from New Delhi.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries