A Paradigm Shift: The Educational Scenario of Healthcare Professionals After the COVID-19 Pandemic
M3 India Newsdesk Nov 18, 2022
This article discusses how the COVID-19 pandemic-related adjustments were evaluated together with future developments and their consequences as the policy was being developed, using the Lancet commission as a baseline.
Introduction
After the onset of the pandemic, the educational scenario for healthcare professionals has taken an absolute turn. With new professional and safety guidelines coming into play, the COVID-19 pandemic has opened up new modes and channels and received and imparted education among health professionals.
The lockdown opened up the most unexpected channels of education like the online mode, which has caused a major shift in the education systems in institutions and they were required to accommodate all these new adaptations for both online and in-person teaching by building more resources and obtaining more technological abilities in order to smoothly facilitate these educational resources to the healthcare professionals.
The Lancet Commission on education for health professionals for the 21st century recommended an interdisciplinary and global approach to review the Flexner century (the century between 1910 to 2010 when the Flexner report and Lancet commission were published respectively. This was done to establish a global integration of healthcare education. The commission identified three types of reforms
- Scientific reforms (providing scientific curriculum in the universities)
- Problem-based learning in academic medical centres
- System-based reforms (developing competencies for effective inter-professional practice in complex healthcare set-ups.
Based on this framework, a health policy was developed which offered a comprehensive set of recommendations. This policy analysed the healthcare education scenario in the past ten years and also analysed the signification developments and changes in the education system before and after the COVID-19 pandemic. The Lancet commission was considered as the baseline for developing the policy but at the same time, future developments and implications of the developments due to the changes brought about by the COVID-19 pandemic were assessed.
Brief description of the health policy
- The annual number of healthcare professionals showed an increase in the past 10 years with the number of doctors being doubled and in the case of nurses and midwives, the number had tripled.
- There was an increase in the number of graduates substantially in higher-income countries and in private schools.
The COVID-19 pandemic restricted the conventional face-to-face and personal-driven learning modules but at the same time, these restrictions facilitated the use of online technologies for continuing education among healthcare professionals. As the pandemic caused an upsurge in utilisation of the healthcare facilities too, there was an urgent need to utilise the online modes of facilitating these healthcare requirements to people through teleconsultation as there were severe restrictions due to the lockdown and this indirectly affected the required competencies by medical professionals The new methods have not yet stabilised but likely to be sustained and in return will create new challenges and opportunities in the field of healthcare education.
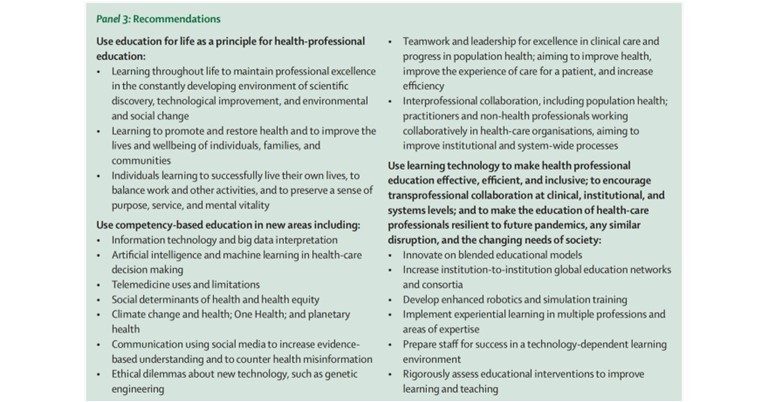
The new education systems will create new technologies based on cognitive sciences and this with open a path for newer innovations.
Development of competency-based education,inter-professional education and information-technology-facilitated education will increase to balance the Flexnerian emphasis on excellence in life sciences with all other perspectives.
Before COVID-19 pandemic
Based on official data sources, the number and various features of medical and public health schools and of graduates in medicine, nursing, or midwifery by country or region were tabulated and also reporting practices like nursing and midwifery graduates were combined despite their distinctive work profile. For public health, only the number of schools was recorded as there are no consistent global data available on the number of graduates, potentially because of heterogeneity among countries in the professional categories included. The cost of education for doctors and nurses was estimated (56 estimates across 47 countries) or indirectly via regression analysis.
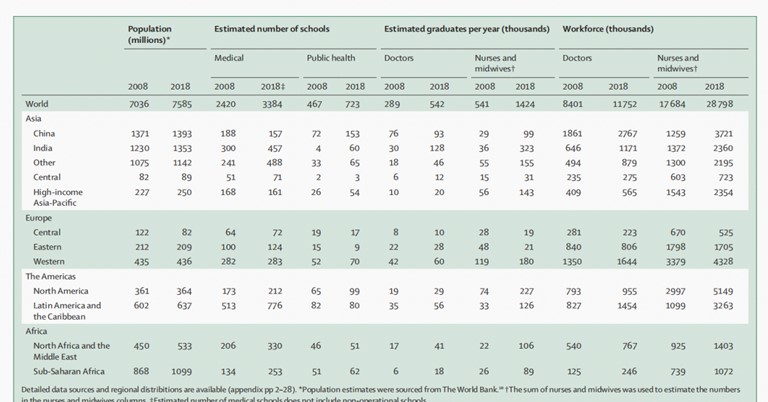
Table 1- The number of medical institutions, graduates and individuals in the healthcare workforce by the region
The number of medical and public health schools has greatly increased. There was also showed a significant doubling in the number of medical graduates and the number of nursing graduates tripled (Table 1). The number of nurses was the majority (59%) of the health professionals, more than all professionals combined together. Eventually, the global distribution of healthcare professionals was imbalanced as there were more healthcare graduates in the higher-income areas as compared to the lower ones.
A systematic analysis done in the past literature which computed data on similar grounds from 204 countries from a period of 1990 to 2019, showed a lot of similarities to the current findings based on this health policy. According to the previous statistics approximately US$110 billion dollars were invested in the education of healthcare workers globally in the year 2018,$60·9 billion was invested in doctors and $48·8 billion was invested in nurses and midwives respectively. These expenditures were higher in North America as compared to Western Europe. (Table 2) describes this data more elaborately with respect to the global scenario.
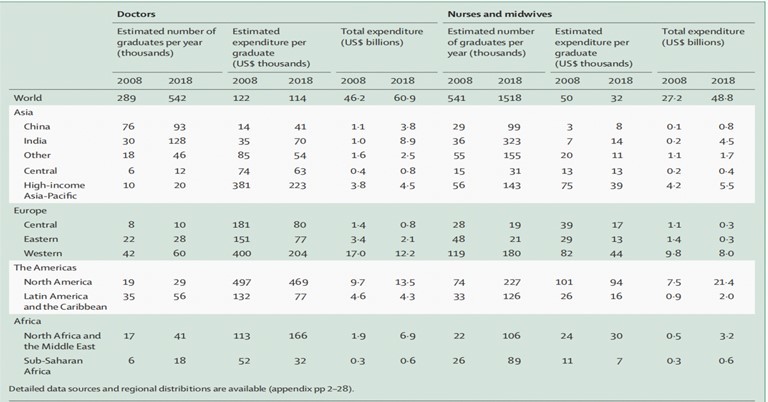
Table 2- Financing of medical and nursing graduates by region
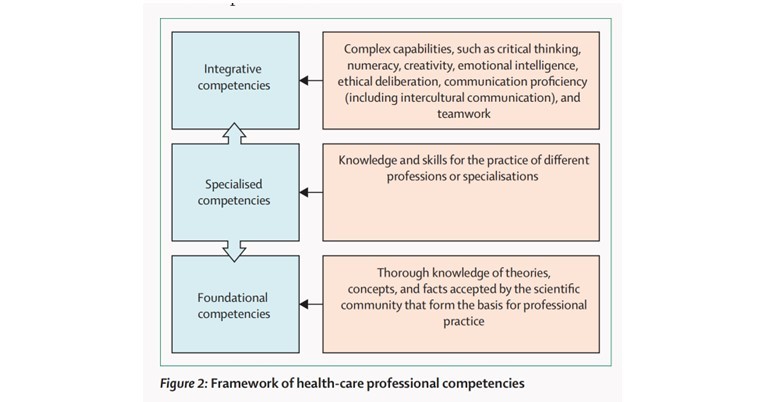
The type of education facilitated to the healthcare workers was entailed under three categories
- Competency-based education-The concept of competency revolves around the ability to have a broad range of abilities in a way where one can combine sharp cognitive skills with other specific skills. This promises more accountability and flexibility in receiving education from the healthcare professionals.
- Inter-professional education- Interprofessional education entails the collaboration of two or more professions to improve the quality of care provided and make the approach more patient-centric. This can be done in multiple healthcare-related disciplines.
- Information technology facilitated the education-The implementation of these technologies in the field of education has been used much before the 2010 Lancet commission was published. Novel approaches like simulation and artificial intelligence can be used in innovative manners for the betterment of medical education.
(Table 3) provides a descriptive analysis of the innovations and categorisation of these three types between 2010 and 2019.
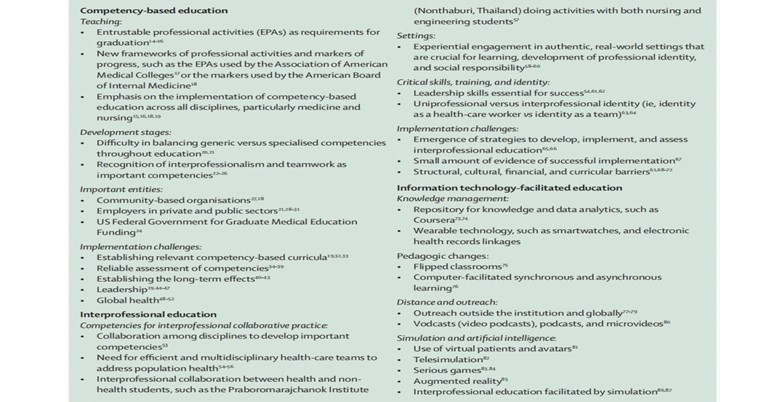
Table 3- Innovations and categorisation of these three types between 2010 and 2019.
During the COVID-19 pandemic
A global survey carried out showed that 80% of the schools and institutes used some kind of information technology-based system to facilitate education as there were restrictions imposed on the routine methods of education. Out of the 67 schools taken for the analysis around 39% used complete online education and around 60% used blended or hybrid forms of education.
There was an upsurge in using online modalities like online learning and simulation in the surgical speciality which constituted 50% from the USA, 25% from Asia and 20% from Europe. There were some major shifts in the education system during the pandemic and those were classified into four domains according to the 2010 Lancet Commission.
- Criteria for admission- Many medical schools switched to online modes of interviews and that allowed them to access a larger number of applicants at the same time. For instance, The University of Houston College of Medicine converted their multiple in-person interviews into online mode. But in a few lower socioeconomic based countries this was a point of bias as their resources were not available
- Competencies- A lot of conventional techniques in some surgical specialities were replaced with modernised and virtual like video learning and surgical simulations
- Methods of teaching-The channels of instruction and teaching were now replaced by an online mode of teaching and a lot of planned conferences, boot camps, virtual sessions and telemedicine features were used to facilitate the same.
- Career pathways- As the pandemic was a grim situation for the world, in a few countries there was an early graduation of the medical professionals to fill in the ever-increasing demands and deficits of the healthcare facilities.
After the COVID-19 pandemic
After the pandemic, there were two important changes were observed:
- The development of new educational technologies and innovations.
- The unprecedented change in the education system due to these new innovations and organisational complexity.
To imbibe this completely, only the initial teaching in medical schools is not enough. Instead one needs to work on building both professional abilities along with personal well-being. The figure below explains the adaption to the new ways and means of healthcare education due to the disruption of the older ones during the pandemic.
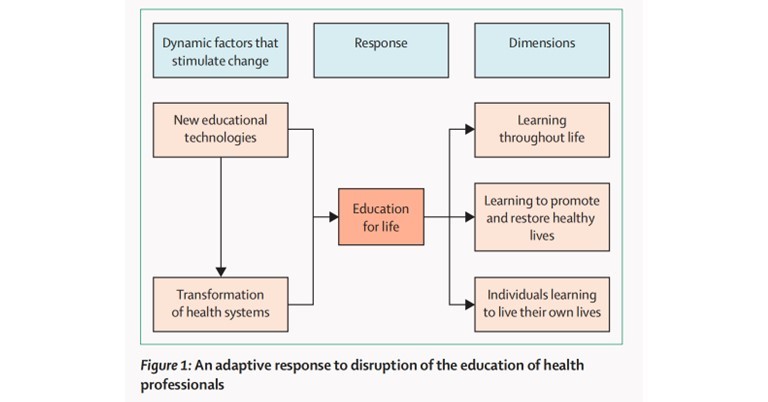
To adapt to the new changes and innovations a newer set of competencies was now required which are categorised into three sections.
- Social justice and health equity-With the newer changes and innovations, it is important to provide larger accessibility of these resources in order to avoid education inequality and social injustice to fewer sections of the world. For example, the Khan academy provided multiple options for online learning to anyone with a basic internet connection as they aimed to eradicate any inequality both for the students and teachers.
- Collaborative approach towards healthcare and education- The COVID-19 pandemic showed a clear picture of healthcare interdependence due to the complexity of the disease and by such future collaborations, there can be global solutions to building a competent healthcare workforce and filling in the needed deficiency.
In a conclusion the health policy made certain recommendations, keeping in mind the future of healthcare education in these changing times after the pandemic.
Key takeaway
The major takeaway after the pandemic was that If an adaptive and resilient healthcare system can be established that is run by competent medical professionals with excellent professional education, it will be much easier to protect and promote all aspects of well-being during and between future pandemics.
Disclaimer- The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Ridima Surve is a practising dentist from Mumbai.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries