Case study of persistent pleural pain misdiagnosed as TB: Dr. Jyotsna Joshi
M3 India Newsdesk Dec 12, 2018
Dr. Jyotsna Joshi, a noted Pulmonologist discusses a case where persisting pleural pain in a patient was misdiagnosed as TB when it was actually pseudomesotheliomatous adenocarcinoma.
Exudative lymphocyte predominant exudates are commonly presumed to be tuberculosis in aetiology and initiated on anti-tuberculosis therapy. However, this leads to misdiagnosis. Such cases should be evaluated further particularly if pleural pain persists.
Case report
A fifty-year-old woman presented with symptoms of three months’ duration of a dry cough, left-sided chest pain and progressive breathlessness. She was previously evaluated with a chest radiograph (CXR) which showed a left-sided large effusion (figure 1) and was empirically treated with anti-tuberculosis therapy (ATT) with no relief of chest pain.
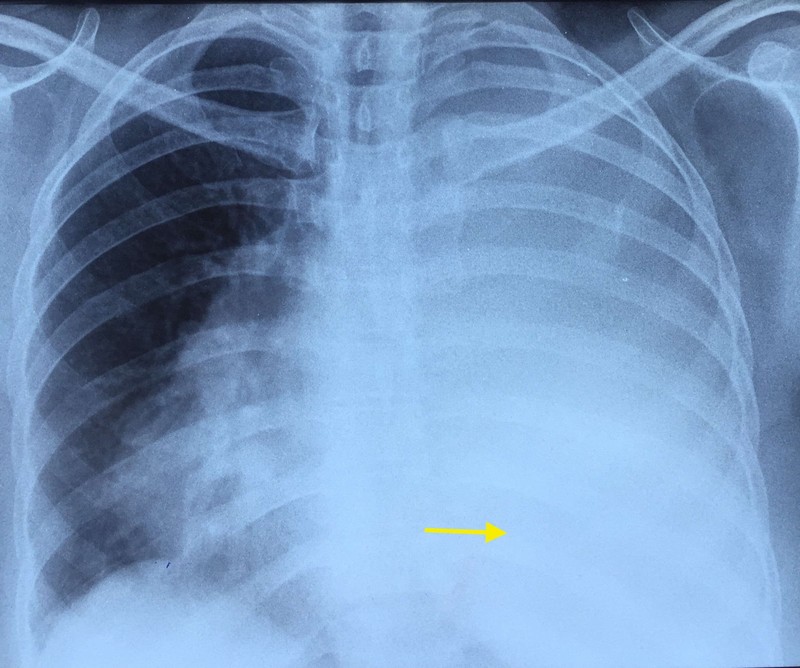
Chest X-ray showing gross left-sided pleural effusion
Examination
The patient was then referred for detailed evaluation and management. On examination, she was afebrile with a pulse of 80 beats per minute, blood pressure of 120/70 mmHg, respiratory rate of 20 cycles per minute, and pulse oximetry saturation of 98% on room air.
Respiratory system examination showed signs of:
- volume loss on the left side in the form of flattening
- depressed shoulder
- reduced spino-scapular distance with dull note
- absent shifting dullness
- decreased breath sounds
- vocal resonance throughout left hemithorax
Other systemic examination was normal. CXR showed pleural thickening.
Q. What should be done next?
A. Contrast-enhanced computed tomography (CECT) of thorax (figure 2A &B)
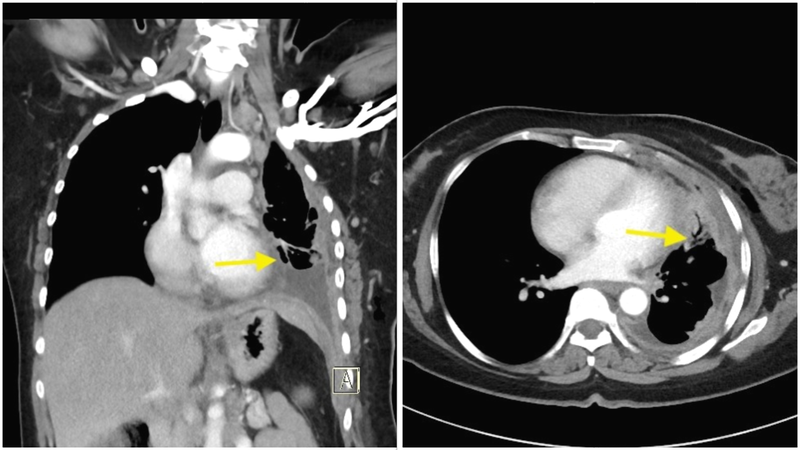
Left: Figure 2A (coronal) & Right: B (axial): Diffuse pleural thickening, thickening of mediastinal pleura and pleural nodularity-Leung's criteria seen
Q. What are the CT findings suggestive of and what next?
A. Malignancy was considered as the diagnosis in view of positive Leung's criteria. We performed an ultra-sonographic guided diagnostic thoracentesis. The pleural fluid was dark yellow, exudative with lymphocyte predominance. The adenosine deaminase (ADA) levels were normal. The pleural fluid glucose was low (35 mg/dl). Pleural fluid analysis for cartridge-based nucleic acid amplification test (CBNAAT) was Mycobacterium tuberculosis (MTB) not detected. Pleural fluid cytology was negative for malignant cells.
Q. What is the next step?
A. In view of her exudative effusion of undetermined aetiology she underwent a closed needle pleural biopsy (CNPB). Pleural biopsy histopathology revealed metastatic adenocarcinoma with positivity for IHC markers of Thyroid Transcription Factor-1 (TTF-1) and Napsin A.
Q. What is the diagnosis?
A. The final diagnosis of pseudomesotheliomatous adenocarcinoma stage IV disease was made. The patient was referred for palliative chemotherapy.
Discussion
Pleural involvement secondary to a carcinoma at a farther site is known however there is a paucity of literature pertaining to its pathogenesis and presentations. The three most frequent tumours to involve the pleura secondarily include lung cancer (35 to 45%), metastatic breast cancer (25%), and malignant lymphoma (10%).
Adenocarcinoma
Adenocarcinoma is the histopathological terminology given to malignancy arising from endocrine or exocrine glands or ducts. They are notorious for their tendency to metastasise widely at an early stage. Adenocarcinoma metastasising to pleura is commonly called as pseudomesotheliomatous adenocarcinoma.
- When it metastasises to the pleura, its clinical, and radiological presentation typically is that of pleural effusion followed by pleural thickening.
- Histopathological and ultrastructural features of this neoplasm closely resemble mesothelioma. The name “Pseudomesotheliomatous adenocarcinoma” stems from this close resemblance.
- Most cases of pseudomesotheliomatous lung cancer are prima facie suspected clinically and radiologically to be mesotheliomas.
- But when the tissue is further evaluated by immunohistochemistry (IHC) or electron microscopy, the pathologic findings indicate that these tumours are not mesotheliomas but are, in fact, primary lung cancers or metastatic cancers growing in a distribution that macroscopically resembles a mesothelioma.
Pseudomesotheliomatous carcinoma
This is a rare variant of peripheral adenocarcinoma of the lung that can manifest with clinical, radiological and pathologic features resembling that of a malignant mesothelioma.
Most "pseudomesotheliomas" arise in the peripheral lung tissue although some can metastasise to the pleura from another site. Radiologically they follow Leung’s criteria of pleural nodularity, circumferential pleural thickening of greater than 1 cm, and thickening of mediastinal pleura.
Besides adenocarcinoma, which accounts for 70% of pseudomesotheliomatous carcinomas, other primary lung cancers, including squamous cell carcinoma, small cell carcinoma, large cell carcinoma, and carcinosarcoma may also present as a pseudomesotheliomatous tumour.
Hence rather than an autonomous neoplasm, pseudomesotheliomas can be said to be a terminology given to a group of malignancies with the common feature of resemblance to mesothelioma; adenocarcinoma is one of them. Differentials to pseudomesotheliomas are epithelial mesothelioma, sarcomatoid mesothelioma and biphasic sarcomatoid mesothelioma.
Pseudomesotheliomatous lung cancers usually present with the same signs and symptoms as diffuse pleural mesotheliomas. The most frequent symptoms are chest pain, dyspnoea, cough, and weight loss. Our patient also presented similar symptoms of a subacute onset and progression.
Pleural Effusions
Pleural effusions are common in both pseudomesotheliomatous lung cancers and pleural mesotheliomas. Pleural fluid in these cases needs to be evaluated further for malignant cells using cytologic, histological, and immunohistochemical examination.
- Our patient was a middle-aged lady and she had never smoked. Hence a consideration of malignancy was low. Tuberculous pleural effusion was less likely owing to the absence of fever and poor response to anti-tuberculosis therapy.
- A persistent pleural pain strongly aroused a suspicion of malignancy.
- The yield of pleural fluid cytology in the diagnosis of pleural malignancies is low and has been variably reported to be 7 to 12%.
- The diagnosis was subsequently confirmed on pleural biopsy histopathology and IHC. The role of a CNPB (cutting needle pleural biopsy) in undiagnosed exudative pleural effusions is established however literature focuses on its major utility in the diagnosis of tuberculosis and its value in the diagnosis of malignant involvement of pleura has been sceptical.
- In our patient, this simple inexpensive bedside investigation played a pivotal role in cinching the diagnosis.
- In case there is no fluid a CT guided fine needle biopsy (FNAB) may be performed.
- Grossly, pseudomesotheliomatous carcinoma presents as a rind of thick, white to tan, firm tissue encasing the lung in a pattern resembling mesothelioma or fibrothorax.
- IHC markers for pseudomesotheliomtous adenocarcinoma commonly found to be positive are Thyroid Transcription Factor-1(TTF-1), Napsin A, Carcinoembryonic Antigen (CEA), LeuM1(CD15), B72.3, Epithelial membrane antigen (EMA) and BerEP4.
Conclusion
Pseudomesotheliomatous adenocarcinoma spreads within the pleural space and presents at a primary tumour classification stage of T3 or with malignant pleural effusion. Patients usually present with advanced disease of stage IIIB or IV and have a poor prognosis, with a mean survival of approximately 7 months.
The prognosis of pseudomesotheliomatous lung adenocarcinoma is similar to that of diffuse epithelioid malignant mesothelioma. Extrapleural pneumonectomy or therapeutic regimens of chemotherapy and/or radiation therapy have been used but are generally ineffective for this advanced form of lung adenocarcinoma. Our patient opted for a palliative chemotherapy.
Therefore, pleural malignancy should be considered as a differential diagnosis of pleural effusion in case pleural pain persists despite therapy in any age group and a simple day care procedure of a pleural biopsy or CT-guided FNAB should be performed to cinch the diagnosis.
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries