Can you prevent heart failure by just diet and exercise?: Prof. Dr. Sundeep Mishra answers
M3 India Newsdesk Mar 07, 2021
This Sunday, we bring to you an article from our archives section. Can something be done to prevent the recurrence of heart failure in patients? Besides clinical intervention, Prof. Dr. Sundeep Mishra in this article mentions the most important aspects of lifestyle recommendations that should be advised to patients to better manage their condition.
For our comprehensive coverage and latest updates on COVID-19 click here.
Heart failure is a big event in life for most persons but it is a disease associated with many myths; it does not literally mean that the heart has failed but simply that the heart in unable to meet the demand placed on it. It is also different from heart attack or heart arrest. It is actually a disease that results from the structural or functional inability of the heart to meet the body’s basic metabolic needs at normal pressures.
In simple terms it is a question of demand and supply mismatch where the heart is unable to meet the demand that is placed upon it. But it is not one single disease but can be result of any of many disorders that affect heart function especially coronary heart disease (including heart attack).
Can something be done to prevent recurrence of heart failure events?
As a matter of fact there are two essential and critically important steps that can be undertaken to prevent the re-occurrence of serious heart failure events. Number one is to take all the prescribed medicines on time. After heart failure, a group of drugs is advised; those which strengthen heart muscle, those that decrease the work of the heart, in addition to other drugs which decrease clotting, lower lipids, or those that control blood pressure or diabetes mellitus that may be required depending on the exact cause of heart failure. Most patients understand the rationale behind the use of these drugs and therefore are very careful to follow the first step.
The second important method to reduce heart failure reoccurrence is lifestyle management. This step is also very important because change in habits can decrease work load upon the heart as also improve its strength. Unfortunately, most patients do not appropriately follow the lifestyle recommendations because:
- They don’t understand its importance in the first place
- Even if they understand the importance they don’t clearly understand/are confused as to what exactly needs to be done?
Below are some of the essential components and tips for lifestyle management after heart attack. There are many false myths associated with diet and exercise in heart failure. One of them is that exercise may be harmful in heart failure. This false myth is so strong that even when repeatedly advised by doctor only ~8% of heart failure patients adhere to an active exercise program (HF-ACTION study).
Diet for heart failure
The importance of diet in heart failure has been recognised since last many years. The cornerstone of nutritional therapy in heart failure prevention and treatment has been restriction of excess sodium intake in order to prevent fluid overload. While sodium remains important, in recent times, macronutrient nutrition has also appeared important in the prevention, particularly there is a role for heart healthy diet because majority of cases of heart failure develop after long-standing coronary heart disease. Healthy dietary patterns high in fruits and vegetables and the inclusion of fish appear important in preventing heart failure, and the benefit of certain dietary supplements (thiamine, Coenzyme Q10) has been suggested.
Salt restriction
Restriction of excess sodium is important in reducing the risk for heart failure. Salt restriction of 2-3 g/day is recommended for heart failure patients but when weather is hot allowance must be made if the patient is sweating. In any case, high salt containing foods and addition of extra salt to prepared foods must be strictly discouraged because high salt intake not only contributes to recurrence of heart failure and increased hospital re-admissions but also increases the need for urgent cardiac transplantation.
Monitoring magnesium status
Magnesium has several benefits for heart failure patients (vasodilator, anti-inflammatory, anti-ischaemic, and anti-arrhythmic). However, due to the use of certain drugs (diuretics) upto ½ the patients may have decrease in serum magnesium. Periodic measurements of magnesium values are essential in heart failure patients and those found deficient should receive its supplementation.
Thiamine supplements for patients treated with diuretics
Certain drugs, particularly furosemide (lasix) are responsible for increasing vitamin B6 (thiamine excretion). If deficient, high-dose thiamine supplementation (300 mg/day) may prove beneficial.
Moderation in alcohol consumption
Moderate alcohol consumption (upto 10 drinks per week) may slightly lower the risk for heart failure but higher dose could be harmful.
Avoidance of saturated fat and fried foods
The risk for heart failure increases with higher amounts of red meat, fried foods and daily consumption of eggs. These food items are also sources of advanced glycation end products, which have been related to the severity of heart failure and are independent predictors for cardiac events in these patients.
Omega-6 to omega-3 fatty acids ratio
The recommended ratio of omega-6 to omega-3 fatty acids in the diet is ≤4:1. However, most diets have a ratio between 10:1 - 50:1. This ratio predisposes individuals to atherosclerosis and inflammation that are often precursors of heart failure. In general, animal foods are rich in omega-6 fatty acids and there is a need to counterbalance it by using plant-based diets which is associated with improvements in major cardiac risk factors. In addition to plant diets, foods specifically rich in omega 3 fats could also be used, like crab, fish (tuna, cod, and salmon), mussels, rapini (Broccoli Rabe), spinach, flax seeds, mangoes, lettuce, and kidney beans. Upto 1600 mg per day is recommended.
Fruits and vegetables
Eating fruits and vegetables decreases the risk of heart failure and therefore eating a minimum of five fruits and vegetables per day is recommended. Interestingly, vegetables seem to be more protective against heart failure than fruits, the intake of ≥5 daily servings fruits and vegetables (combined) can decrease the risk by 1/5th.
Healthy diet pattern
Both Mediterranean (rich in salads, olive oil, and nuts) and DASH (sodium restriction) style diets, as well as diets with lower meat content, higher unsaturated fat and those higher in fish, can contribute to lower risk of heart failure.
Coenzyme Q10 supplementation
Coenzyme Q10 can improve heart function (stroke volume, cardiac output, cardiac index, and end-diastolic volume) in patients with heart failure, irrespective of aetiology (idiopathic, dilated, ischaemic, hypertension, valvular heart disease, and congenital heart disease). A dose of 300 mg Coq10 per day can reduce deaths and hospital admissions in patients with heart failure.
Exercise in heart failure
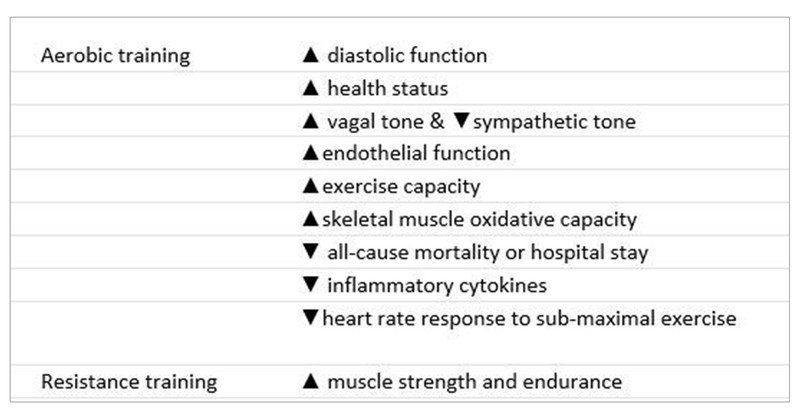
While there is a feeling that exercises may be harmful in patients with heart failure, the reality is that a balanced exercise regimen consistently leads to improvement in exercise capacity, symptoms and quality of life and decreases hospital stay and mortality in these patients. Pathophysiologically, there could be several benefits of exercise on heart failure (Table 1). The benefit has been demonstrated with moderate-intensity exercise (60-70% peak heart rate), although a training effect has also been demonstrated after ≤3 months of low-intensity training (40 to 50% peak VO2).
Training considerations
The standard recommendations for exercise training in general include aerobic activity performed at least 30 minutes, ≥5 days/week, with specific parameters that define exercise intensity, duration, and frequency.
Exercise intensity is a matter of some controversy and while an intensity range of 70 to 80% of peak heart rate determined from a symptom-limited exercise test or simply calculated as 220-age can be used, a moderate-intensity target of 60 to 70% heart rate can be safer (especially among post-infarction heart failure).
Modality of training is another consideration. Although aerobic exercise remains the mainstay of clinical training programs, later, resistance training can also be employed as it also has some benefits (improved muscle strength, endurance, and blood flow associated with a lower VO2 at sub-maximal workloads).
Table 1: Benefits of exercise training in heart failure
This article was originally published on September 25, 2020.
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
The author, Dr. Sundeep Mishra is a Professor of Cardiology.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries