Behavioural Management by Non Pharmacological Means
M3 India Newsdesk Oct 03, 2024
Behaviour management in a dental office refers to methods of obtaining a child’s approval for treatment on a dental chair based on communication, and patient/ parent education with empathy, coaching and listening. This article covers the factors and classification of behaviour management techniques.
Treating a child instead of just doing dental work is the idea underlying behaviour guidance. Behaviour management is how the dental health team effectively and efficiently performs treatment for a child and at the same time, instils a positive dental attitude (Wright, 1975).
Objectives of behaviour management (Snowder, 1980)
- To establish effective communication with the child and parent.
- Gain child and parent confidence for dental treatment.
- Teach children positive aspects of preventive dental care.
- Provide a comfortable, relaxing environment for the child.
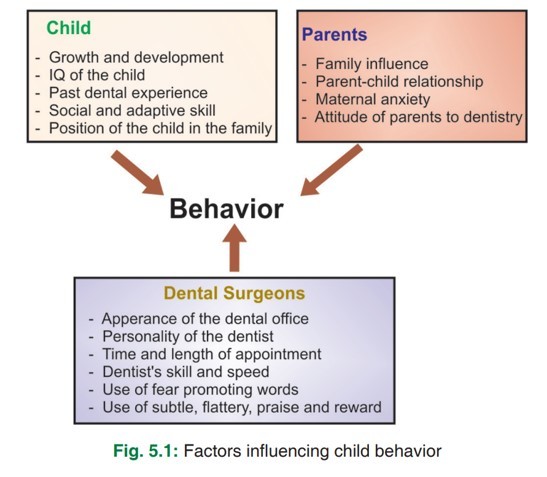
Factors influencing child’s behaviour
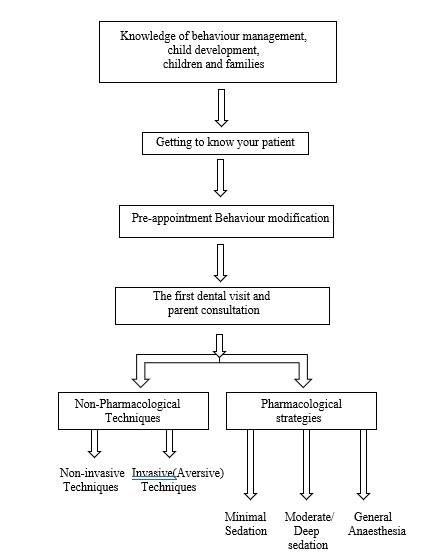
Classification of behaviour management techniques
A. Psychological approach
- Preappointment behaviour modification
- Communication
- Use of a second language
- Tell, show, do
- Tender love care
- Desensitisation
- Contingency management
- Visual imagery
- Modelling
- Behaviour shaping
- Assimilation and coping
- Hypnosis
- Retraining
- Distraction
- Externalisation
- Parental presence or absence
- Reframing
- Voice control
B. Physical approach
- Hand over mouth
- Physical restraints
C. Pharmacological
- Premedication
- Conscious sedation
- General anaesthesia
Preappointment behaviour modification
A. Audiovisual modelling
- The goal is to reproduce the behaviour exhibited by the model.
- The child sees a video cassette before proceeding to the dental clinic, on the day of the appointment.
- The type of model can be siblings, other children or parents.
- It is best recommended to use the model of the same.
Advantages
- Stimulation of new behaviour
- Facilitation of behaviour in a more appropriate manner
- Elimination of inappropriate behaviour because of fear
- Extinction of fear
B. Preappointment mailing
- Contact the child’s parents before the first dental visit.
- Preparing the patient for the first dental visit increases the likelihood of success.
- Parents can be contacted by telephone as a reminder the day before the dental appointment.
Communication
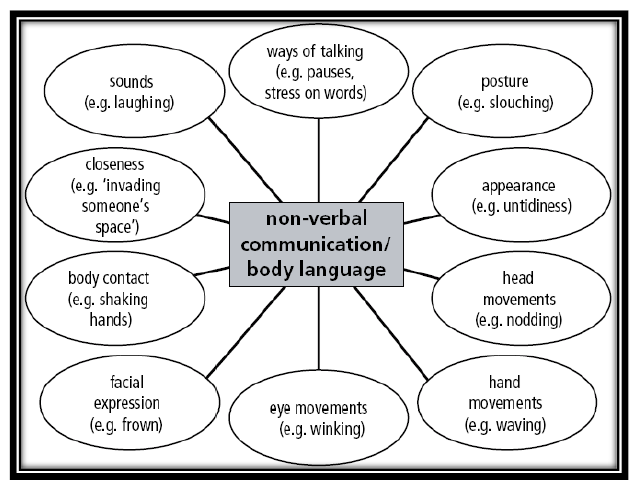
There are 2 ways of establishing communication: Verbal & Nonverbal
Verbal communication (Use of Euphemisms)
Euphemisms should be used such as:
- Xray: photo
- Xray machine: camera
- Rubber dam: raincoat
- Air rotor: whistle
- 3way syringe: air water gun
- Suction: vacuum cleaner
Tell-Show-Do(TSD)
- By Addleston in 1959.
- It is the most effective technique.
- The child is told about the procedure in a language and words understandable to the child. Then child is shown instruments and materials and a way of performing the treatment(approximation). When the child becomes assured and relaxed, treatment is completed.
Various modifications of the concept of TSD have been introduced recently:
- Tell-Play-Do (TPD)
- Tell–Show-Play-Doh
Ask-tell-ask
- It involves inquiring about the patient’s visit and feelings toward or about any planned procedures (ask).
- Explaining procedure through demonstrations and non-threatening language(tell).
- And again inquiring if the patient understands and how the child feels about treatment (ask).
Objectives
- Examine any anxiety that can cause non-compliant conduct while receiving treatment
- Teach the patient about the procedures and their implementation
- Confirm the patient is comfortable with treatment before proceeding
Desensitisation
- By James and popularised by Wolpe.
- It means to take away one's sensitivity to a type of behaviour. This is used in children having pre-established fears and uncooperative behaviour.
Modelling
- Based on Bandura’s social learning theory, states that one’s learning or behaviour acquisition occurs through observation of a suitable model performing a specific behaviour.
- It is used to eliminate or minimise the fear of dentistry in children by allowing children to observe an older sibling undergoing dental treatment.
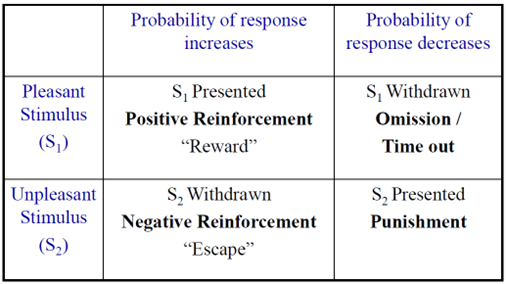
Contingency management
- Based on BF Skinner’s operant conditioning.
- Contingency management is the process of presenting positive reinforcers or removing negative reinforcers.
There are 3 Types of reinforcements:
- Social (praise, handshake, pat, hug)
- Material (gift, toys and not sweets)
- Activity (watching TV shows, cartoons)
Externalisation
The process by which a child’s attention is focused away from sensation associated with dental treatment by involvement in verbal or dental activity.
Objectives
- To decrease the perception of unpleasantness
- To interest and involve children
Distraction
- A more recent approach to behaviour control lowers anxiety by diverting the patient's attention from the sounds and/or visuals of dental procedures.
- Objective relax the patient and reduce anxiety during treatment.
- Use stories and fairy tales.
- Use slow instrumental music.
- The sound of music will eliminate unpleasant dental sounds like the sound of a handpiece.
There are two types of distractions:
A. Active distraction
- Interactive toys
- Guided imagery
- Controlled breathing and relaxation
- Virtual reality
B. Passive distraction
- Audio: listening to music
- Audio-visual: watching television
Memory restructuring
Behavioural approach in which memories associated with negative or difficult events (e.g., first dental visit, local anaesthesia, restorative procedure, extraction) are restructured into positive memories using information suggested after the event has taken place.
Restructuring involves four components:
- Visual reminders (photo of a child smiling at first visit).
- Positive reinforcement through verbalisation.
- Concrete examples to encode sensory details.
- Sense of accomplishment.
Retraining
Designed to fabricate positive values and to replace negative behaviour
Approaches
- Avoidance (e.g. avoid extensive pulp therapy with pulp capping)
- De-emphasis and substitution (e.g. substitute high-speed handpiece with spoon excavator)
- Distraction (e.g. distract the child with stories/activities/audiovisual aids)
Flooding technique
A technique that eliminates the child’s attempts to avoid experiences that he perceives to be undesirable, e.g. Hand over mouth(HOM), physical restraints.
Voice control
- By Pinkham in 1985.
- Sudden and firm commands are given to gain the child’s attention.
Objectives
- To gain patient attention and compliance
- To avoid negative behaviour
- To establish authority
Contraindications
Children who due to age, disability, or mental or emotional immaturity are unable to understand.
Reframing
It is defined as “taking a situation outside the frame up to that moment containing the individual in different conditions and visualise(reframe) it in an acceptable manner to the person involved and with this reframing, both the original threat and the threatened solution can be abandoned”
Hypnosis
By Franz A Mesmer in 1773.
Uses
- To reduce nervousness and apprehension
- To eliminate defence mechanisms that patients use to postpone dental work
- To control functional or psychosomatic gapping
- To prevent thumb sucking and bruxism
- To induce anaesthesia
Hand-over-mouth technique
By Dr Evangeline Jordan in 1920.
Objectives
- Gain the child’s attention by enabling communication with the dentist
- Eliminate inappropriate avoidance behaviour to dental treatment
- Increase child’s confidence
- Assure child safety
Variations of the techniques: Airway uninstructed, hand over both nose and mouth(HOMAR), towel held over mouth only, dry towel over nose and mouth, wet towel over nose and mouth.
Protective stabilisation
Restriction of patient’s freedom of movement, with or without patient’s permission, to decrease risk of injury while allowing safe completion of treatment.
Equipments:
For limbs:
- Posey strap
- Posey vest
For body:
- Pedi wrap
- Papoose board
For mouth
- Mouth props
- Tongue blades
Objectives
- To reduce or eliminate unwanted movement.
- Protect patient, staff, dentist or parent from injury.
- Facilitate delivery of quality dental treatment.
Indications: In the patient who requires immediate diagnosis, urgent care, and treatment.
Contraindications: Patients associated with medical, psychological, or physical conditions.
Precautions:
- Patient’s medical history- reviewed carefully.
- Tightness and duration of stabilisation must be monitored at regular intervals.
- Stabilisation around extremities or the chest must not restrict respiration.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr Neha Kalantri is a practising dentist from Nashik.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries