Article: Using CGM Data to Enhance Patient Outcomes
M3 India Newsdesk Apr 07, 2025
One of the most promising technological advancements in diabetes care is Continuous Glucose Monitoring (CGM). This tool allows us to gain real-time insights into patients' glucose patterns, offering a much more nuanced and effective way to manage blood glucose levels than traditional methods.

As a physician, managing patients with diabetes presents both challenges and opportunities for improvement in their quality of life. Continuous Glucose Monitoring CGM empowers both patients and clinicians to make more informed decisions, improving patient outcomes in various ways.
The Role of Continuous Glucose Monitoring (CGM)
Continuous Glucose Monitoring (CGM) is a technology that provides a constant, real-time stream of data on glucose levels, typically through a small sensor placed under the skin. Unlike traditional blood glucose meters, which offer a single measurement at a point in time, CGM offers continuous data, usually in 5-minute intervals. This gives a clearer picture of a patient's glucose patterns, including fluctuations that may not be captured through traditional testing methods.
The primary aim of CGM is to provide actionable data that can lead to better glycemic control and ultimately improve patient outcomes. The real-time data helps to:
- Identify Periods of Hypo- and Hyperglycemia: Detecting low or high blood glucose before it becomes symptomatic enables earlier intervention.
- Guide Insulin Therapy: Clinicians can adjust basal and bolus insulin regimens based on the data from CGM, leading to better control and fewer complications.
- Improve Patient Education: By showing how lifestyle choices (such as diet, exercise, or medication adherence) impact glucose levels, patients are empowered to make better decisions.
Clinical Reasoning Behind the Use of CGM
- The clinical reasoning behind CGM use is simple: Patients with diabetes have highly variable glucose levels due to multiple factors, including food intake, stress, activity levels, and medications.
- Traditional fingerstick testing provides a snapshot of glucose levels at one point in time, but it fails to capture the full range of fluctuations, including postprandial spikes or nocturnal hypoglycemia.
- These fluctuations can contribute to long-term complications, such as retinopathy, nephropathy, neuropathy, and cardiovascular diseases, even when average glucose levels (A1c) seem well-controlled.
- CGM allows for a more detailed understanding of glucose dynamics over time, enabling clinicians to intervene before significant complications arise.
Case Study
Case Study 1: Managing Type 1 Diabetes in a Young Adult
Patient Profile:
A 25-year-old female, diagnosed with Type 1 Diabetes (T1D) at age 12, presents with complaints of frequent hypoglycemic episodes, particularly in the middle of the night. Her current A1c is 7.2%, but she has difficulty with consistent glucose control, and her overnight glucose levels often dip below 70 mg/dL, causing her to wake up feeling fatigued and anxious.
Clinical Approach:
Given her symptoms of nocturnal hypoglycemia, I decided to start her on CGM. Upon analysing her CGM data over several days, we discovered that her glucose levels would often spike after dinner and then fall precipitously in the late evening, resulting in hypoglycemia around 3 AM. This pattern had gone undetected through conventional fingerstick testing.
Using the CGM data, we were able to adjust her insulin regimen. The patient was instructed to decrease her evening rapid-acting insulin by 20% and to have a small, balanced snack before bed. Additionally, we explored the use of a basal insulin pump to provide more precise insulin delivery throughout the night.
Outcome:
After making these adjustments, the patient reported a significant reduction in nocturnal hypoglycemia. Her average overnight glucose levels stabilised, and she experienced fewer disruptions to her sleep. Her A1c remained well-controlled at 7.1%, but the elimination of nocturnal hypoglycemia improved her quality of life and reduced anxiety around overnight glucose drops. The use of CGM provided real-time insights into her glucose patterns, which would have been impossible to identify through intermittent fingerstick testing.
Case Study 2: Improving Glycemic Control in an Older Adult with Type 2 Diabetes
Patient Profile:
A 68-year-old male with Type 2 Diabetes (T2D) has struggled with maintaining target glucose levels despite adherence to oral medications and lifestyle modifications. His A1c has been hovering around 8.5%, and he frequently experiences fatigue and occasional dizziness, which he attributes to fluctuating glucose levels. However, his healthcare provider has not been able to identify specific glucose patterns using conventional methods.
Clinical Approach:
Given his reports of symptoms, I recommended CGM to assess his glucose variability. His CGM data revealed significant postprandial glucose spikes, particularly after lunch, when his glucose levels peaked at over 250 mg/dL before gradually returning to baseline in the evening. Despite this, his fasting glucose levels were within normal limits, and his A1c remained elevated due to the frequent postprandial excursions.
We decided to adjust his treatment regimen, adding a short-acting insulin regimen to control the post-meal glucose spikes. We also discussed meal timing and composition, recommending smaller, more frequent meals with a greater emphasis on fiber and protein to help prevent large glucose swings.
Outcome:
After initiating the insulin adjustments and meal modifications, the patient's postprandial glucose spikes were significantly reduced, and his overall glucose variability decreased. Within three months, his A1c dropped to 7.3%. His energy levels improved, and he reported feeling less fatigued and dizzy. Importantly, the CGM data enabled us to tailor his treatment plan to his specific needs, something that would not have been possible with traditional monitoring alone.
Practical Applications for Clinicians
The two case studies above illustrate how CGM can provide actionable insights that lead to improved patient outcomes. However, integrating CGM into clinical practice requires careful consideration of several factors:
1. Patient Selection
Not all patients require CGM, and it is essential to identify the right candidates. CGM is most beneficial for patients with:
- Type 1 Diabetes (T1D) and insulin-treated Type 2 Diabetes (T2D) who need more frequent glucose monitoring.
- Unstable glucose patterns or frequent hypoglycemia.
- Difficulty achieving target A1c despite adherence to standard therapies.
2. Data Interpretation and Decision Making
One of the challenges of using CGM is interpreting the data and translating it into actionable clinical decisions. CGM data can be overwhelming, and it is easy to become fixated on individual data points. However, it is crucial to focus on trends, such as:
- Time in Range (TIR): The percentage of time the patient spends within the target glucose range (typically 70-180 mg/dL). Increasing TIR is associated with a reduction in complications.
- Glucose Variability: High variability in glucose levels, even with a reasonable average, may contribute to complications over time.
- Hypoglycemia/Hyperglycemia Alerts: Patients with frequent hypo- or hyperglycemic events should have their therapy adjusted to reduce these occurrences.
3. Patient Education
It is essential to educate patients on how to use the CGM data effectively. Patients should understand how food, exercise, and insulin therapy affect their glucose patterns and be encouraged to make adjustments based on the real-time data provided by CGM. This may involve teaching patients how to recognise trends and adjust their lifestyle or therapy to achieve better control.
Take-home Message
CGM represents a significant advancement in diabetes care. From my perspective as a clinician, it provides an unparalleled level of insight into patients' glucose dynamics, allowing for more precise treatment adjustments and personalised care. The case studies presented above demonstrate the profound impact that CGM can have on patient outcomes by identifying glucose fluctuations that may otherwise go unnoticed. By using CGM data, we can help patients achieve more stable glucose levels, reduce complications, and improve their overall quality of life. For clinicians, CGM is an invaluable tool that complements clinical judgment and empowers both patients and healthcare providers to achieve better diabetes management.
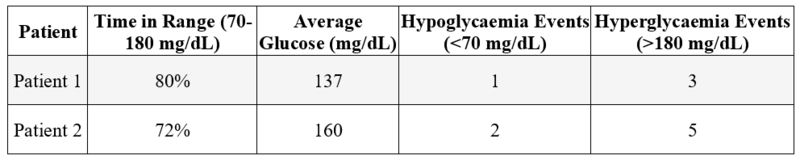
Table 1: Example CGM Data Interpretation
By integrating CGM into routine care, physicians can help patients achieve more consistent glucose control, which is essential for preventing long-term complications and improving overall health outcomes.
Disclaimer: The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
About the author of this article: Dr. Akshayaa is a General Practitioner at Sri. Balaji Heart Centre, Chennai.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries