Antibiotics for treating common infections: ICMR guidelines
M3 India Newsdesk May 26, 2022
A step-by-step rationalised guide on the use of antibiotics in the treatment of common infections along with the list of the antibiotics by ICMR is penned down in this article.
Antimicrobial resistance prevalence in India
Antimicrobial resistance (AMR) is a worldwide public health emergency. In India, AMR is progressively increasing in prevalence across a variety of pathogens, posing a danger to our capacity to treat and cure common diseases.
Antibiotic irrationality, uncontrolled over-the-counter sales of antibiotics, and a lack of advice and understanding about antibiotic usage are all significant contributors to AMR occurrences. Inadequate monitoring and improper use of antimicrobials have a significant role in the development and spread of AMR.
To address this rising issue, India's finest infectious disease specialists and clinical microbiologists from prestigious medical organisations created evidence-based treatment recommendations for common diseases. This will serve as practical guidance for health care workers in terms of antimicrobial treatment and correct use.
The antibiotic susceptibility data included in these guidelines are from selected premier tertiary care facilities in India and do not reflect any particular community statistics.
Antimicrobial resistance data is known to vary across various healthcare institutions and between different clinical sections of the same institute. Hence each healthcare organisation and each clinical department must modify their respective guideline appropriately utilising ICMR guidelines as a reasonable structure.
Five objectives of these recommendations
- To raise antimicrobial resistance knowledge and comprehension
- To increase monitoring and research
- To minimise the prevalence of infection
- To optimise the use of antimicrobials
- To secure long-term investment in the fight against antimicrobial resistance
In India, doctors prescribe antibiotics arbitrarily, they are distributed without a prescription over the counter. As a result, a sustained effort at all levels is essential to avoid antimicrobial resistance propagation.
Antibiotics: A step-by-step rationalised guide
Step 1: Establishing a clinical diagnosis rather than depending just on fever, procalcitonin levels, WBC counts, cultures, or radiography to establish an infection diagnosis.
Step 2: Restricting empiric antibiotic treatment to individuals who are critically sick.
Step 3: Become familiar with your bugs - Identify potential sources of illness and predict potential microbial diseases
Step 4: Select the proper antibiotic
Step 5: De-escalation/modification of treatment regimen based on culture and antimicrobial susceptibility data, as well as patient status
Step 6: In the following clinical conditions, discontinue antibiotics-
I. Respiratory tract syndromes
- Viral pharyngitis
- Viral rhinosinusitis
- Viral bronchitis
- Non-infectious cardio-pulmonary syndromes misdiagnosed as pneumonia
II. Skin and soft tissue infections
- Subcutaneous abscesses
- Lower extremity stasis dermatitis
III. Asymptomatic bacteriuria and pyuria including in catheterized patients
IV. Microbial colonization and culture contamination
V. Low-grade fever
Step 7: Shorten the length of treatment
The following durations are suggested by practice guidelines and recommendations for the optimal length of treatment for different infectious illness conditions:
- Community-acquired pneumonia: 5 days
- Hospital-acquired pneumonia: 8 days
- Skin and Soft tissue infections: 5 days
- Urinary tract infections
- Cystitis: 3-5 days
- Pyelonephritis: 5-14 days
- Catheter-associated: 7 days
- Staphylococcal aureus bacteraemia – low risk of complications = 2 weeks
- High risk of complications: 4-6 weeks
- Intra-abdominal infection: 4-7 days
- Surgical antibiotic prophylaxis: 1 dose
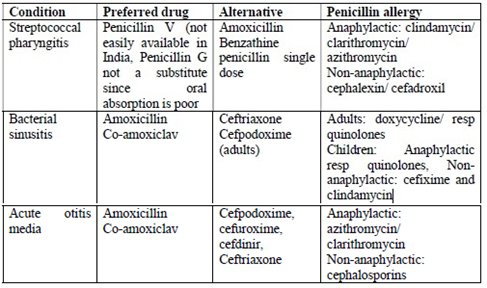
Antimicrobial therapy in URTI
Antibiotics for some of the commonly encountered infections in clinical practice are summarised below as per ICMR recommendations.
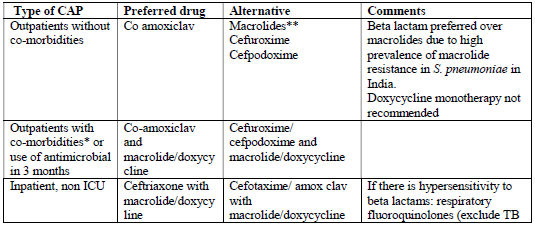
Choice of empiric antimicrobial therapy in adult community-acquired pneumonia
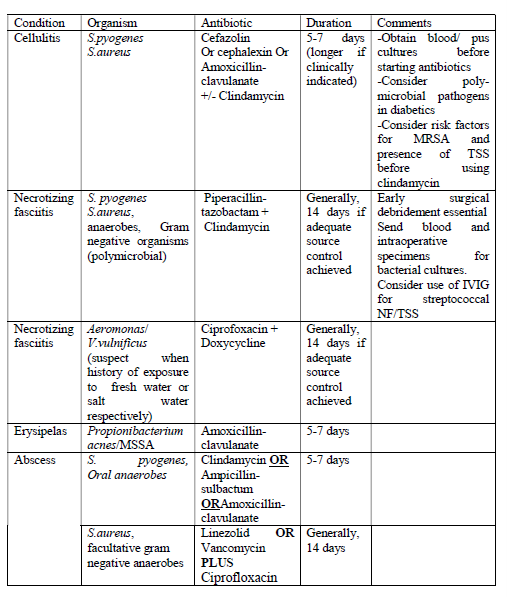
Antibiotics guidelines for skin and soft-tissue infections (SSTIs)
Click here to see references
Disclaimer- The views and opinions expressed in this article are those of the author's and do not necessarily reflect the official policy or position of M3 India.
The author is a practising super specialist from New Delhi.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries