Age Related Macular Degeneration
M3 India Newsdesk Dec 10, 2024
This article focuses on ARMD and explains its classification, clinical impact, and risk factors while reviewing diagnostic tools and modern treatment strategies. It elaborates on research on advanced therapies to address unmet needs in Dry and Wet ARMD management.
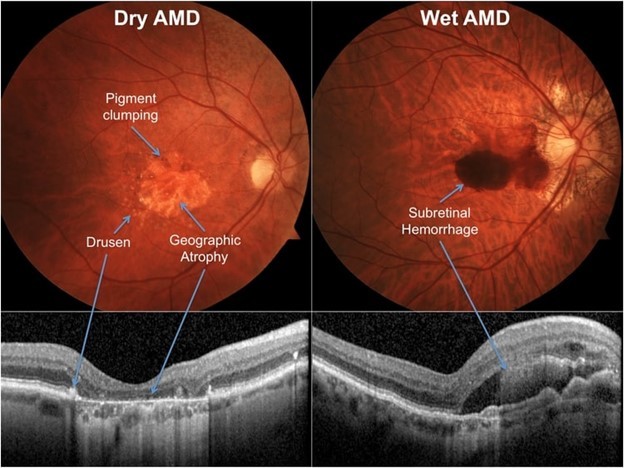
Age-related macular degeneration (ARMD) is a leading cause of central visual impairment among individuals over the age of 55. It is the most common cause of acquired blindness in European adults and has a significant prevalence in India and the United States, with rates ranging from 1.4% to 3.1% in India. ARMD remains the primary cause of vision loss in people aged 60 and above. This condition manifests in two major forms: Dry ARMD and Wet ARMD.
Dry ARMD is characterised by the presence of drusen, which are deposits that accumulate between the retina and the retinal pigment epithelium (RPE), leading to progressive atrophy of the RPE and the overlying photoreceptors.
In contrast, Wet ARMD involves the formation of abnormal blood vessels beneath the retina, a process known as choroidal neovascularisation. This can result in leakage of blood or fluid, causing rapid and severe vision loss. Advanced stages of both forms can result in significant retinal damage, including subretinal haemorrhages, fluid accumulation, and fibrosis.
Although genetic factors, especially among those of European descent, play a substantial role in ARMD development, environmental factors such as smoking, diet, and ageing also contribute. Given the lack of effective treatments for Dry ARMD, the exploration of novel therapeutic strategies has become a focal point of ongoing research.
Types and characteristics of ARMD
A hallmark feature of ARMD is the presence of drusen, which are yellowish deposits located at the level of the RPE. Drusen can be part of the normal ageing process, but their size and quantity are directly related to the risk of developing ARMD. Drusen are categorised based on their size:
- Small drusen are less than 65 microns in diameter.
- Intermediate drusen measure between 65 and 125 microns.
- Large drusen are greater than 125 microns in diameter.
Early ARMD is characterised by the presence of multiple small or intermediate drusen without significant vision loss. As the condition progresses to intermediate ARMD, there are numerous intermediate and large drusen present, often accompanied by pigmentary changes in the RPE. Advanced ARMD involves severe retinal damage, including geographic atrophy of the RPE or the development of disciform scars.
Risk factors for ARMD
- The risk of developing ARMD increases with age, with a marked rise in incidence after the age of 55.
- Smoking is a significant modifiable risk factor, as it has been shown to double the risk of developing ARMD.
- Genetic factors also play a crucial role, with variants in the Complement Factor H (CFH) gene and other complement system components being strongly associated with the condition.
- Systemic conditions such as hypertension, cardiovascular disease, hyperlipidaemia, diabetes, obesity, and hypermetropia have also been linked to an increased risk of ARMD.
- The pathological sequence of ARMD typically begins with the accumulation of drusen, which can lead to serious detachment of the RPE. This process may progress to RPE atrophy and subsequent sub-RPE proliferation, eventually resulting in the formation of choroidal neovascular membranes and disciform scars, significantly impairing central vision.
Clinical manifestations
Patients with ARMD often present with a gradual loss of central vision, which can lead to blurred vision, especially when reading or performing tasks that require fine visual acuity. They may also experience metamorphopsia, where straight lines appear wavy or distorted, and micropsia, where objects appear smaller than they are.
Central scotomas, or blind spots, are common, particularly as the disease progresses. Near vision and the ability to perceive fine detail are often the most affected, significantly impacting daily activities.
Pathogenesis
- The pathogenesis of ARMD involves a complex interplay of genetic, environmental, and biochemical factors. Oxidative stress is a major contributing factor, leading to the accumulation of reactive oxygen species that damage retinal cells.
- Inflammation, particularly complement-mediated inflammation, plays a significant role, with many complement system proteins found within drusen deposits.
- Lipofuscin, a byproduct of photoreceptor degradation, accumulates in the RPE and contributes to oxidative damage. Abnormal lipid metabolism also exacerbates drusen formation.
- MicroRNA dysregulation has been linked to the development of ARMD, offering potential targets for future therapeutic interventions.
Diagnosis
- Diagnosis of ARMD typically begins with a clinical fundus examination, where the presence of drusen and other retinal changes can be observed.
- The Amsler grid test is a simple yet effective tool for detecting visual distortions, metamorphopsia, and scotomas. Fundus photography is used to document and monitor the progression of retinal changes.
- Advanced imaging techniques, such as fundus autofluorescence (FAF), can provide insights into the health of the RPE. Fluorescein angiography (FFA) and Indocyanine green angiography (ICG) are used to detect and evaluate choroidal neovascularisation.
- Optical coherence tomography (OCT) and OCT angiography provide detailed cross-sectional images of the retina, helping to identify fluid accumulation, retinal thinning, and structural changes.
Management strategies
According to the Age-Related Eye Disease Study 2 (AREDS2), supplementation with antioxidants and minerals can help slow the progression of intermediate to advanced ARMD. The recommended supplements include:
- 500 milligrams of Vitamin C
- 400 International Units of Vitamin E
- 80 milligrams of zinc oxide
- 2 milligrams of copper as cupric oxide
- 10 milligrams of lutein and 2 milligrams of zeaxanthin
- The exclusion of beta-carotene is advised to reduce the risk of lung cancer in smokers
Treatment of neovascular ARMD
The mainstay of treatment for Wet ARMD includes anti-VEGF (vascular endothelial growth factor) therapy, which involves intravitreal injections of drugs like Ranibizumab, Aflibercept, and Brolucizumab. Another approach is the use of anti-angiopoietin factors, such as Faricimab, which targets additional pathways involved in neovascularisation. Photodynamic therapy (PDT) with verteporfin is another treatment option that selectively targets abnormal blood vessels without damaging surrounding retinal tissue.
1. Advanced therapies/novel therapies
- As we now understand different pathogenesis for ARMD, like Oxidative injury, complement-mediated damage to retinal cells, inflammatory substances like tyrosine Kinase and abnormal Lipid metabolism can lead to the development of ARMD. Newer treatment strategies revolve around modifying these causative factors.
- Emerging therapies for ARMD include complement system inhibitors like Pegcetacoplan, which targets complement factors implicated in dry ARMD. It is given through the intravitreal route and it inhibits the C3b pathway. This is an FDA-approved drug.
- Another drug, Avacincaptad Pegol, targets complement factor 5 and has been approved for geographic atrophy associated with Dry ARMD. It is also for intravitreal injection and is FDA-approved.
- New pharmacological approaches also include tyrosine kinase inhibitors and angiostatic steroids, though their long-term effectiveness and safety profiles are still under evaluation.
- Among Angiostatic steroids, Anecortave acetate is used as a Scleral depot for wet ARMD and indicated in wet ARMD as effective for 6 months but is currently not approved by the FDA
- Tyosin Kinase inhibitors can be used via the oral route, downregulating VEGF receptors common drugs in use are Imatinib, Vorolanib, lapatinib, and Vatalanib, But not FDA-approved to date.
- Another novel drug CT1812( Kaftrio) is under research for use in Dry ARMD, currently used for Cystic fibrosis, But ocular indications are under trial
- Gene therapy represents a promising alternative to ongoing anti-VEGF injections, aiming to enable the eye to produce its own anti-VEGF. Techniques involve either a surgical subretinal injection or a routine intravitreal injection.
2. Surgical and cellular therapies
- In cases of severe retinal damage, surgical options like vitrectomy can be considered. For patients with central scarring, macular translocation surgery may be an option.
- Stem cell-based therapies, such as RPE stem cell transplantation, are being actively researched as potential treatments for Dry ARMD. These approaches involve layering stem cells on scaffolds and transplanting them into the retina to replace damaged cells.
3. Visual rehabilitation
For patients experiencing significant vision loss, visual rehabilitation plays a critical role. Low vision aids, including magnifiers, high-power reading glasses, and telescopic lenses, can help maximise remaining vision.
Advanced wearable vision enhancement devices, such as IrisVision and eSight, offer hands-free magnification, improving visual acuity and contrast sensitivity. The Implantable Miniature Telescope, approved by the FDA, can be a viable option for patients with bilateral late-stage ARMD, offering enhanced magnification and improved quality of life.
The rising prevalence of ARMD, driven by increasing life expectancy and an ageing global population, underscores the need for continued research into novel treatment strategies. While current therapies cannot fully reverse ARMD, they can slow disease progression and help preserve vision. Advances in gene therapy, complement pathway inhibitors, and cellular therapies hold promise for the future, potentially transforming the management of ARMD. With ongoing innovation in visual aids and assistive technologies, patients can maintain a higher quality of life, even as the search for curative treatments continues.
Disclaimer- The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policy or position of M3 India.
The author of this article: Dr Vandana Jain is an Ophthalmologist from Indore.
-
Exclusive Write-ups & Webinars by KOLs
-
Daily Quiz by specialty
-
Paid Market Research Surveys
-
Case discussions, News & Journals' summaries